#hydrogels
Implantable microrobots: Innovative manufacturing platform makes intricate biocompatible micromachines
A team of researchers led by Biomedical Engineering Professor Sam Sia at Columbia Engineering has developed a way to manufacture microscale-sized machines from biomaterials that can safely be implanted in the body. Working with hydrogels, which are biocompatible materials that engineers have been studying for decades, Sia has invented a new technique that stacks the soft material in layers to make devices that have three-dimensional, freely moving parts. The study, published online January 4, 2017, in Science Robotics, demonstrates a fast manufacturing method Sia calls “implantable microelectromechanical systems” (iMEMS).
By exploiting the unique mechanical properties of hydrogels, the researchers developed a “locking mechanism” for precise actuation and movement of freely moving parts, which can provide functions such as valves, manifolds, rotors, pumps, and drug delivery. They were able to tune the biomaterials within a wide range of mechanical and diffusive properties and to control them after implantation without a sustained power supply such as a toxic battery. They then tested the “payload” delivery in a bone cancer model and found that the triggering of release of doxorubicin from the device over 10 days showed high treatment efficacy and low toxicity, at 1/10 of the standard systemic chemotherapy dose.
Post link
A new gel helps wounds heal
Researchers from UCLA have developed an injectable hydrogel that helps skin wounds heal faster.
The new synthetic polymer material creates an instant scaffold, sort of like stacked gumballs, that allows new tissue to latch on and grow within the cavities formed between linked spheres of gel.
Conventionally, ointments and other hydrogel dressings have been used to fill in wounds to keep the areas moist and accelerate healing. But none of the materials used now provide a scaffold to allow new tissue to grow while the dressing itself degrades. As a result, the new tissue growth is relatively slow and fragile.
So bringing about an injectable biomaterial that promotes rapid regeneration of tissue has been a “holy grail” in the field of tissue engineering, said co-principal investigator Dino Di Carlo.
They envision the material being useful for a wide variety of wound application, including lacerations to large-area burns.
UC Berkeley researchers have also been developing new approaches to tissue engineering. Last March, their advancement in “herding cells” marked a new direction for smart bandages.
Post link
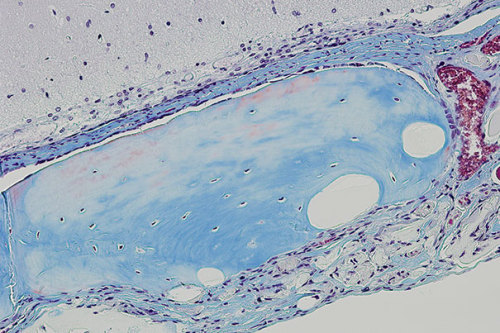
New Porous Hydrogel Could Improve the Success of Stem Cell Tissue Regeneration
Using a new porous hydrogel, scientists have experimentally improved bone repair by boosting the survival rate of transplanted stem cells and influencing their cell differentiation.
Possible stem cell therapies often are limited by low survival of transplanted stem cells and the lack of precise control over their differentiation into the cell types needed to repair or replace injured tissues. A team led by David Mooney, a core faculty member at Harvard’s Wyss Institute, has now developed a strategy that has experimentally improved bone repair by boosting the survival rate of transplanted stem cells and influencing their cell differentiation. The method embeds stem cells into porous, transplantable hydrogels.
In addition to Mooney, the team included Georg Duda, a Wyss associate faculty member and director of the Julius Wolff Institute for Biomechanics and Musculoskeletal Regeneration at Charité – Universitätsmedizin in Berlin, and Wyss Institute founding director Donald Ingber. The team published its findings in today’s issue of Nature Materials. Mooney is also the Robert P. Pinkas Family Professor of Bioengineering at the Harvard John A. Paulson School of Engineering and Applied Sciences.
Stem cell therapies have potential for repairing many tissues and bones, or even for replacing organs. Tissue-specific stem cells can now be generated in the laboratory. However, no matter how well they grow in the lab, stem cells must survive and function properly after transplantation. Getting them to do so has been a major challenge for researchers.
Post link