#alcoholic liver disease
Pathogenesis
Stage One
- Ethanol is metabolised in the liver toacetaldehydeby alcohol dehydrogenase
- which is in turn metabolised to acetate by aldehyde dehydrogenase.
- As acetaldehyde is formed, NAD is metabolised to NADH as a cofactor in this reaction.
- ThisNADH inhibits the actions of isocitrate dehydrogenase and alpha ketoglutarate and fatty acid oxidation, meaning it favours fatty acid synthesis.
- Fat builds up in vacuoles of hepatocytes and mitochondria begin to dysfunction under oxidative stress, creating reactive oxygen species.
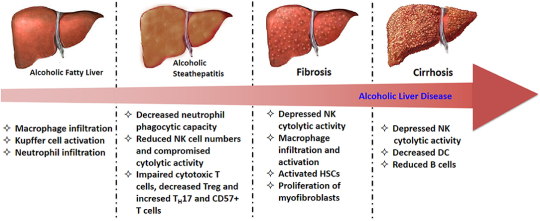
- This fatty stage is known as steatosis and is stage one of alcoholic liver disease. It is reversible.
Stage Two
- Inflammatory cytokines such as IL-6 and TNFa influx in, causing inflammation.
- Water begins to accumulate inside hepatocytes and they begin to balloon. This causes significantcholestasis.
- The inflammatory cytokines stimulate hepatocytes to produce collagen, which can begin to formfibrosis.
- This collagen can be pericellular or around central veins, forming collagen bridges. This is a precursor for cirrhosis.
Stage Three
- As the fibrosis progresses,hepatocytes begin to die and cirrhosis occurs.
- This is end-stage alcoholic liver disease and can lead to liver failure and death.
Liver function tests
- Instage 1; all LFTs will be raised. AST and ALT will be raised by approximately 5-10x the upper reference limit except albumin. They will both usually be below 300IU/L. AST will be raised above ALT; this is different to other hepatic conditions such as cholestasis, tumours, hepatitis, where ALT will be above AST.
- In stage 2; ALP and bilirubin will increase significantly as cholestasis occurs and blocks bile duct. This will usually be above 300IU/L, which is different from filtrative diseases, where ALP is usually raised to 200-250IU/L. AST and ALT may increase further.
- Instage 3; AST and ALT are between 10-100x the upper reference limit, suggesting significant cirrhosis and damage to cells. AST will remain above ALT. GGT will be raised significantly, which is common with alcoholic liver disease. Albumin will be decreased, suggestive of total liver failure. In other hepatic conditions, liver damage usually does not reach this stage and so albumin stays within the range.
