#epiglottitis
Pediatrics (neonates to school age; adolescence is another topic) is probably my least favorite specialty to deal with and they are one of the hardest to help at times with all the elements that go with the patient. Whether it is dealing with the sick child or the distraught parents, we must sift through the physical findings and the information from the parents to understand what is going on. This gets especially sticky when it comes to some upper airway complications in the younger group.
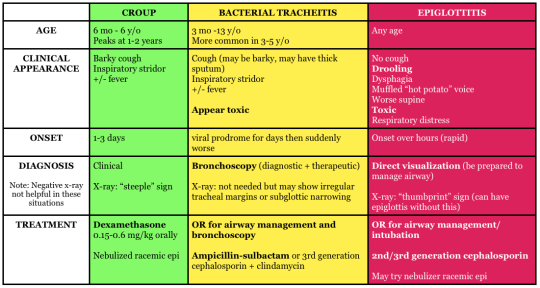
Two very common upper airway problems in the younger populations include Croup and Epiglottitis. Both can be dangerous, but require different management when treatment is concerned. This article will give you a brief overview of the pathophysiology, signs and symptoms, treatments, and key points to remember.
Croup
Pathophysiology: Commonly a viral infection (RSV, adenovirus, influenza A and B, etc.) of the upper respiratory system for ages 6 to 36 months. Major inflammation has occurred in the larynx, trachea, bronchi, bronchioles, and lung parenchyma; causing obstruction of the airway. As the swelling progresses supraglottic the patients with begin show signs of respiratory distress. Further along, the patient’s lower airway may begin to begin having atelectasis, due to the lack of air keeping the alveoli open.
Croup is a slow progression of inflammation. Noticing early that the patient has upper respiratory issue is key in the management. Due to the smaller airway of children, we must not hesitate to seat
Signs and Symptoms: The most common sign of croup will be the seal like bark with inspiratory stridor. With this means that the patient is in respiratory distress and quickly heading to failure. If you hear the seal like bark, check the lower lung fields for crackles, because possible atelectasis may have begun.
Commonly more serious during night, awakening them from sleep. Other signs to know include:
- Tachypnea
- Retractions
- Cyanosis
- Shallow respirations
- Fever
Treatment: Emergency treatment for croup is a humidified air and a dose of corticosteroids. If in further destress, racemic epinephrine will assist with edema. ETCO2 and O2 readings will help determine if there is retention of gasses, which may lead to acidosis. ABGs will be needed to confirm this as well.
Usually, patients will be able to return home to be monitored. Family should watch for difficulty breath and be using humified air. Antipyretics will assist in keeping fevers down as well.
Epiglottitis
Pathophysiology: Influenza type B, streptococcus pneumoniae or aureus may cause epiglottitis. The epiglottis is a small flap above the glottic opening, which is used to prevent foreign objects entering the trachea. When the epiglottis is infected, with will swell, narrowing the airway for the patient. Increased work of breathing may occur and soon my might have a patient in respiratory failure.
Epiglottitis is a more acute problem, with sudden onset and quick changes to mentation form the restriction of airflow.
Signs and symptoms: As the epiglottis swells, the child may begin to develop stridor. When stridor occurs, we must ask the question is this an object or is this medical. Other signs that might point you towards epiglottitis will be:
- Sore throat
- fever
- Odynophagia
- Drooling
- Irritability
- Cyanosis
- Tripoding or nasal flaring
Treatment: The most important thing with these patients is to ensure they have an airway. Do not try and examine the patient, especially if you are a paramedic on scene (Load and go). When gathering a medical history, it is especially important to ask for vaccination in the pediatric population. Today, Influenza vaccinations are given to children, but we do have a set population now that do not vaccinate their children. X-rays of neck will be done and a visual examination may be performed. Keep the patient calm at this time, further agitation may cause the airway to swell more.
Patient will commonly receive an antibiotic, such as ceftriaxone, to help with the bacteria. ET tubes may be places in severe cases and usually remain for 24 to 48 hours. Trachostomes may be required, if a ET tube cannot pass the glottic opening.
Key Points
- Both Croup and Epiglottitis can be dangerous to pediatric patients. If you have a child that has stridor and any signs of distress, they will need immediate attention.
- Out of hospital, assume epiglottitis and rule it out when you can. This load and go for you
- Croup X rays may show steeple sign, but epiglottitis won’t
Written by: MEDDAILY
Join me on Facebook!
