#meddaily
Pediatrics (neonates to school age; adolescence is another topic) is probably my least favorite specialty to deal with and they are one of the hardest to help at times with all the elements that go with the patient. Whether it is dealing with the sick child or the distraught parents, we must sift through the physical findings and the information from the parents to understand what is going on. This gets especially sticky when it comes to some upper airway complications in the younger group.
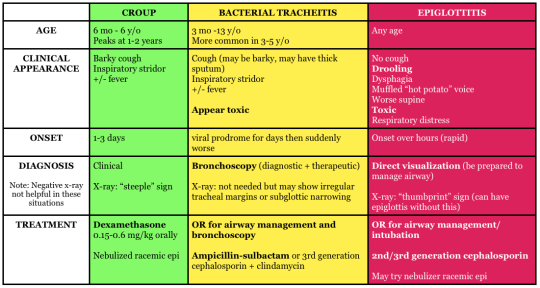
Two very common upper airway problems in the younger populations include Croup and Epiglottitis. Both can be dangerous, but require different management when treatment is concerned. This article will give you a brief overview of the pathophysiology, signs and symptoms, treatments, and key points to remember.
Croup
Pathophysiology: Commonly a viral infection (RSV, adenovirus, influenza A and B, etc.) of the upper respiratory system for ages 6 to 36 months. Major inflammation has occurred in the larynx, trachea, bronchi, bronchioles, and lung parenchyma; causing obstruction of the airway. As the swelling progresses supraglottic the patients with begin show signs of respiratory distress. Further along, the patient’s lower airway may begin to begin having atelectasis, due to the lack of air keeping the alveoli open.
Croup is a slow progression of inflammation. Noticing early that the patient has upper respiratory issue is key in the management. Due to the smaller airway of children, we must not hesitate to seat
Signs and Symptoms: The most common sign of croup will be the seal like bark with inspiratory stridor. With this means that the patient is in respiratory distress and quickly heading to failure. If you hear the seal like bark, check the lower lung fields for crackles, because possible atelectasis may have begun.
Commonly more serious during night, awakening them from sleep. Other signs to know include:
- Tachypnea
- Retractions
- Cyanosis
- Shallow respirations
- Fever
Treatment: Emergency treatment for croup is a humidified air and a dose of corticosteroids. If in further destress, racemic epinephrine will assist with edema. ETCO2 and O2 readings will help determine if there is retention of gasses, which may lead to acidosis. ABGs will be needed to confirm this as well.
Usually, patients will be able to return home to be monitored. Family should watch for difficulty breath and be using humified air. Antipyretics will assist in keeping fevers down as well.
Epiglottitis
Pathophysiology: Influenza type B, streptococcus pneumoniae or aureus may cause epiglottitis. The epiglottis is a small flap above the glottic opening, which is used to prevent foreign objects entering the trachea. When the epiglottis is infected, with will swell, narrowing the airway for the patient. Increased work of breathing may occur and soon my might have a patient in respiratory failure.
Epiglottitis is a more acute problem, with sudden onset and quick changes to mentation form the restriction of airflow.
Signs and symptoms: As the epiglottis swells, the child may begin to develop stridor. When stridor occurs, we must ask the question is this an object or is this medical. Other signs that might point you towards epiglottitis will be:
- Sore throat
- fever
- Odynophagia
- Drooling
- Irritability
- Cyanosis
- Tripoding or nasal flaring
Treatment: The most important thing with these patients is to ensure they have an airway. Do not try and examine the patient, especially if you are a paramedic on scene (Load and go). When gathering a medical history, it is especially important to ask for vaccination in the pediatric population. Today, Influenza vaccinations are given to children, but we do have a set population now that do not vaccinate their children. X-rays of neck will be done and a visual examination may be performed. Keep the patient calm at this time, further agitation may cause the airway to swell more.
Patient will commonly receive an antibiotic, such as ceftriaxone, to help with the bacteria. ET tubes may be places in severe cases and usually remain for 24 to 48 hours. Trachostomes may be required, if a ET tube cannot pass the glottic opening.
Key Points
- Both Croup and Epiglottitis can be dangerous to pediatric patients. If you have a child that has stridor and any signs of distress, they will need immediate attention.
- Out of hospital, assume epiglottitis and rule it out when you can. This load and go for you
- Croup X rays may show steeple sign, but epiglottitis won’t
Written by: MEDDAILY
Join me on Facebook!
There is quite a lot to be said about the medications we use for patients with arrhythmias. It’s easy to get lost as to what drugs do what and how, but thankfully there was a kind enough person by the name of Vaughan Williams, who actually broke them down into separate classes. Each class effects separate parts of the cardiac cycle, ultimately changing the electrical current of the heart.
Cardiac Action Potential
Before looking at the medications, we have to understand the cardiac cycle and how it actually works.

Source:x
The above chart presents the four phases of an action potential in a ventricular myocardial cell and how the electrolytes are used to cause the depolarization and repolarization of myocardial cells.
Phase 0 begins with a slight influx of sodium until it passes the potential threshold. Once past the threshold, more sodium channels will open and flood the cell, causing it the depolarize.
Phase 1 is an efflux of potassium from the cell, causing the cell to reach 0mV.
Phase 2 happens at this point. This is when calcium influx happens, prolonging the repolarization period. This period also goes by the name of an absolute refractory period for the cell, since it cannot depolarize during this time.
Phase 3 Calcium channels close again and potassium continues to efflux from the myocardial cell until the internal cell voltage returns to -90mV. Majority of potassium channels then close and the heart enters phase 4, which potassium is allowed to continue to leak into from the cell.
This process happens anywhere from 60 to 100 times per MINUTE!
Vaughan Williams Classifications
The major purpose of the medications in this class effect they way the cardiac action potential works in the cells of the heart. The drugs usually help to slow down specific phase to the heart and allow the heart to fix itself a bit.
Class I - Sodium Channel Blockers
These medications are designed to disrupt phase 0, causing a prolongation of it. There are 3 subcategories (a,b,c) that are broken down into moderate, weak, and strong.
This article won’t go into great depths, but the major goal of the class is to prolong the QRS complex and prolong or shorten QTi.
Medications include:
Lidocaine
Verapamil
Procainamide
Propafenone
Class II - Beta Blockers (-olol or -alol)
Quite commonly used out of hospital for patients with hypertension, beta blockers are actually a common antidysrhythmic. The basic pharmacology is: by blocking the beta-1 receptor sites, it prevents stimulation of the cardiac muscle to beat faster. The increase of sympathetic tone will decrease the rate the heart will beat.
Medications include:
- Propranolol
- Metoprolol
- Carvedilol
Class III - Potassium Channel Blockers
Similar to the Class Ia medications, potassium channel blockers are used to prolong APD, which can cause a prolongation of ERP. This class of medication is commonly known to treat different ventricular dysrhythmias (Vtach or Vfib). The most common medication for this class is Amiodarone and deserves a post of its own.
It’s most common use is during CPR, when the patient is in pulses Vtach or Vfib rhythm and is then followed by a drip with ROSC is achieved. An important note to make about Amiodarone is it can take 16 weeks to leave the system.
Medications include:
- Amiodarone
- Sotalol
- Ibutilide
Class IV - Calcium Channel Blockers
Commonly uses for Afib with RVR and PSVT, a calcium channel blocker will prolong phase 2 of the action potion in the cell. The goal is to slow the conduction through the atrioventricular (AV) node, slowing the ventricular tachycardia that is occurring. By prolonging the ERP in the AV node, the heart is able to regulate the rate better.
Calcium channel blockers are commonly prescribed by physicians to assist in the care of such arrhythmias. One side effect of these drugs is it may drop the patient’s BP, so ensure you have an SBP >100 or a MAP >65, prior to administering the medication
Class V - Others
This is the mix bag class. These drugs do not truly fit in any category but are still highly important to mention anyways. Two of these medications are Adenosine and Digoxin.
Adenosineprevents the re-entry of a signal in a sinus rhythm, preventing SVT. A warning though is for patients that have WPW syndrome may cause an increase in heart rate instead, so make sure you’re reading the rhythm correctly.
Digoxineffects vagal tone and is seen less as an emergency drug and more as a maintenance drug for chronic heart issues. A major issue with this drug is it holds a very narrow therapeutic index. Toxicity is quite possible if given too much.
Summary
Each class works in its own way on the action potential in the cardiac conduction system. How they affect the heart greatly determines when and how the medication should be used in different medical scenarios. The point of this article is to help a bit with the pharmacodynamics involved with the medications and to hint at the situations a person in the medical field would use them?
Remember to check out my facebook page. Feel free to send suggestions for possible article ideas, it might pop up some time. Always remember that medicine is an art, just as much as a science.
