#endocrinology
Comprehensive Care for Gestational Diabetes
Women with diabetes need comprehensive care before and during pregnancy. The Diabetes and Pregnancy Program (DAPP) at UC San Diego Health, the only one of its kind in the San Diego Region, cares for the diverse population of women with diabetes in San Diego County.
DAPP is designed to provide specialized care to patients with diabetes through a multidisciplinary approach, following the California Diabetes and Pregnancy Program guidelines.
“Patients with type 1 or type 2 diabetes, or those who have recently been diagnosed with gestational diabetes, require a team of specialists to assist with a healthy pregnancy and optimize the outcome for both the patient and baby,” said Sandy Ramos, MD, director of DAPP and perinatologist at UC San Diego Health.
“For example, working with a specialist to manage blood sugar before and during pregnancy can decrease the risk of complications and make it more likely that the patient can carry the baby to term.”
Ramos and Kristen Kulasa, MD, endocrinologist at UC San Diego Health, elaborate:
Question: How common is gestational diabetes and what are the complications?
Answer: Approximately one in five women delivering babies in San Diego County begin their pregnancies with diabetes, and others develop gestational diabetes during pregnancy. These women are at risk for complications during pregnancy and after delivery, including high blood pressure, eye disease, kidney disease, too much weight gain, severe hypoglycemia (low blood sugar) and diabetic ketoacidosis (DKA).
Their babies are also at increased risk for complications, including macrosomia (high birth weight), higher rates of miscarriage and stillbirth, birth defects, delivery complications and jaundice.
Q: What type of services does DAPP provide?
A: DAPP includes six certified diabetes care and education specialists (DECS), nutritionists and social workers under the direction of two maternal fetal medicine experts. The program provides care to approximately 500 patients with gestational diabetes, 120 patients with type 2 diabetes and 40 patients with type 1 diabetes per year.
As a clinical program in the region’s only academic medical center, DAPP provides leading edge diabetes care from preconception to postpartum, utilizing the latest technology available, including the use of sophisticated insulin pumps and continuous glucose monitoring.
For example, the DAPP team has found success using “closed loop systems” to improve glucose control in patients with type 1 diabetes in pregnancy. This technology allows integration of information from the continuous glucose monitor to augment or “talk” to insulin pumps. This allows the insulin pump to increase insulin delivery if the glucose values are high or to decrease or even suspend insulin delivery if the glucose value is low.
With the aim of improving the maternal and neonatal outcomes of women with diabetes, patients are also given the opportunity to participate in clinical trials, such as the Medical Optimization of Management of Pregnancy with Overt Diabetes (MOMPOD) trial, a randomized clinical trial of Metformin as an adjunct to insulin for the treatment of type 2 diabetes.
DAPP provides primary obstetrical care for complicated patients with diabetes and is able to provide consultative services to co-manage patients with gestational diabetes.
Q: How are you addressing gestational diabetes with patients in terms of lifestyle interventions and medications available?
A: To treat gestational diabetes, we encourage nutrition changes to limit simple carbohydrates and recommend exercise. Most patients with gestational diabetes can manage their glucose values with these changes alone. If elevations persist, they can be treated with medicines like insulin and metformin. However, these lifestyle changes are important tools to continue to lower the risk of development of type 2 diabetes. Women who develop gestational diabetes have a higher risk of developing type 2 diabetes later in life.
Q: What research needs to be done to improve how diabetes is managed in pregnancy?
A: There are many new medications used for management of type 2 diabetes that haven’t been studied in pregnancy. The issue of safety of these medications needs further exploration in pregnancy. Additionally, technology, including blue tooth-enabled meters and continuous glucose monitors, commonly used in type 1 diabetes, need to be studied in other types of diabetes in pregnancy to see if they may be useful tools to improve the care of women with diabetes.
— Michelle Brubaker
Post link

Discovery of new metabolic pathway for stored sugars helps explain how cellular energy is produced and expended in obesity, advancing therapeutic potential
Humans carry around with them, often abundantly so, at least two kinds of fat tissue: white and brown. White fat cells are essentially inert containers for energy stored in the form of a single large, oily droplet. Brown fat cells are more complex, containing multiple, smaller droplets intermixed with dark-colored mitochondria — cellular organelles that give them their color and are the “engines” that convert the lipid droplets into heat and energy.
Some people also have “beige” fat cells, brown-like cells residing within white fat that can be activated to burn energy.
In recent years, there has been much effort to find ways to increase brown or beige fat cell activity, to induce fat cells, known as adipocytes, to burn energy and generate heat in a process called thermogenesis as a means to treat obesity, type 2 diabetes and other conditions.
But the therapeutic potential of brown fat — and perhaps beige fat cells —has been stymied by the complexity of the processes involved. It wasn’t until 2009 that the existence of active brown fat cells in healthy adults was confirmed; previously it was believed they were common only in newborns.
In a new study, published online October 27, 2021 in Nature, an international team of researchers led by senior author Alan Saltiel, PhD, director of the Institute for Diabetes and Metabolic Health at University of California San Diego School of Medicine, describe how energy expenditure and heat production are regulated in obesity through a previously unknown cellular pathway.
Image: Artistic rendering of a brown fat cell with nucleus in pink, mitochondria in purple and yellow lipid droplets scattered throughout. Image courtesy of Scientific Animations.
“Sweet! How Glycogen is Linked to Heat Generation in Fat Cells”
Excess Neuropeptides Disrupt Lung Function in Infant Disease and COVID-19
Excess fluid in the lung can significantly disrupt lung function and gas exchange, but researchers at University of California San Diego School of Medicine were surprised to find that neuropeptides may be to blame.
In a study published March 17, 2022 in the journal Developmental Cell, scientists show that excessive neuropeptide secretion by neuroendocrine cells in the lungs can lead to fluid buildup and poor oxygenation. However, blocking the neuropeptide signals with receptor antagonists prevented the leakage and improved blood-oxygen levels, suggesting that neuropeptides may be a promising therapeutic target for conditions marked by excess lung fluid.
This mechanism was discovered in the context of neuroendocrine cell hyperplasia of infancy (NEHI), a lung disease affecting infants in which lung size and structure appear normal but blood-oxygen levels are consistently low. Its defining feature is an increase in the number of pulmonary neuroendocrine cells (PNECs), but until now, physicians did not know how these cells contributed to the disease.
In the new study, researchers confirmed that PNECs and their neuropeptide products are the drivers of NEHI, but also showed that PNEC numbers were increased in the lungs of COVID-19 patients with excess lung fluid. This suggests a similar mechanism may contribute to COVID-19 symptoms.
The study was led by Xin Sun, PhD, professor of pediatrics at UC San Diego School of Medicine and the Division of Biological Sciences.
“We were surprised to find that neuropeptides can play such a major role in gas exchange,” said Sun. “Researchers are just starting to appreciate the relationship between the nervous system and the lungs, but the more we understand it, the more we can modulate it to treat disease.”
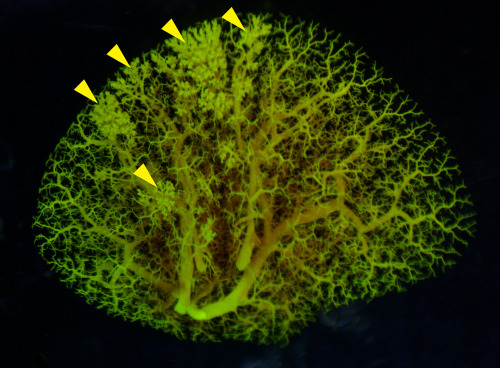
Pictured above: An angiogram of blood vessels in the NEHI mouse lung shows multiple sites of fluid leakage, marked by yellow arrowheads.
— Nicole Mlynaryk, Bigelow Science Communication Fellow
Post link
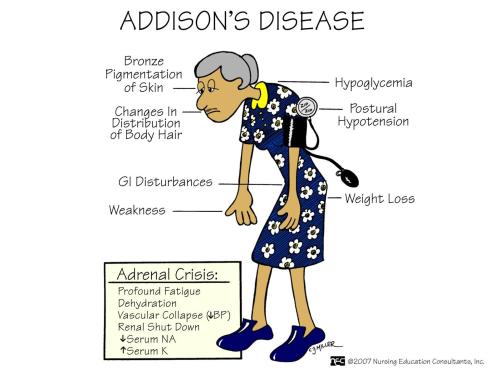
Addison’s Disease.
Addison’s disease is a rare but known disorder (John Fitzgerald Kennedy suffered from it) and it is also referred to as adrenal insufficiency. Adrenal insufficiency develops when adrenal glands do not produce enough of the hormone cortisol. This can happen due to a problem within the adrenals (called Addison’s disease or primary adrenal insufficiency) or due to a problem with ACTH, the signal the brain sends to the adrenals instructing them to make cortisol (called secondary adrenal insufficiency).
An important distinction for patients is that people with primary adrenal insufficiency (Addison’s disease) usually don’t make enough of the hormone aldosteronetoo; so in addition to taking cortisol replacement, they also need aldosterone replacement. Also, ACTH levels are elevated. People with secondary adrenal insufficiency are only low on cortisol.
Causes: Primary adrenal insufficiency - the outer layer of the adrenal glands is called the adrenal cortex. If the cortex is damaged, it may not be able to produce enough cortisol. A common cause of primary adrenal insufficiency is an autoimmune disease that causes the immune system to attack the adrenal gland(s). There are some very rare syndromes (several diseases that occur together) that can cause autoimmune adrenal insufficiency, such as Autoimmune Polyendocrine Syndrome (type 1 or type 2). Other causes include: amyloidosis; bleeding into the adrenal glands; cancer that spreads to the adrenal glands; infections (bacterial, fungal, tuberculosis) of the adrenal glands; surgical removal of the adrenal glands. Secondary adrenal insufficiency - it is caused by a lack of ACTH, made in the pituitary gland. By far the most common cause of this type of adrenal insufficiency is chronic steroid use.
Signs and symptoms:
- Weakness
- Fatigue
- Abdominal pain
- Nausea
- Weight loss
- Low blood pressure
- Increased pigmentation of the skin, including areas not exposed to the sun (due to high levels of ACTH in primary adrenal insufficiency. This occurs because melanocyte-stimulating hormone (MSH) and ACTH share the same precursor molecule, pro-opiomelanocortin (POMC))
- Salt craving (due to low levels of aldosterone in primary adrenal insufficiency)
- Postural Hypotension
- Depression
Treatment: it involves replacing the cortisol and/or aldosterone that the body is not able to produce, or that it secretes in an insufficient quantity. Cortisol is replaced with an oral synthetic glucocorticoid. The drug is taken one or two times each day. Aldosterone is replaced with an oral mineralcorticoid.
Post link
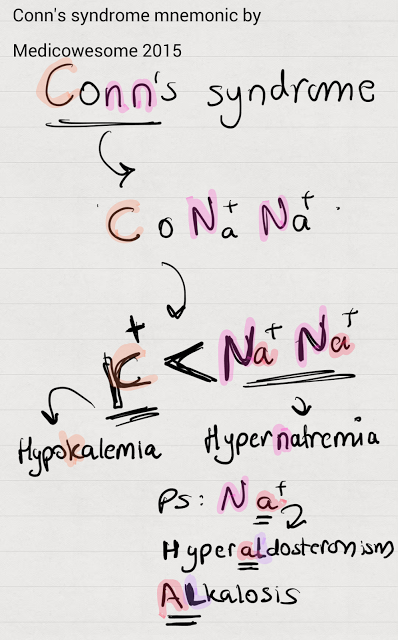
Conn’s syndrome mnemonic
Hi. I keep forgetting that Conn’s syndrome is hyperaldosteronism. Can you help me out with this?
Sure! :D
The N’s are for sodium - Hypernatremia!
The C makes a K for potassium, which is less than the number of N’s, therefore, hypokalemia!
Also, Na+ is sodium. A could remind you of Aldosterone.
AL could remind you of ALkalosis.That’s all!
-IkaN
Post link
Conn’s syndrome mnemonic
Hi. I keep forgetting that Conn’s syndrome is hyperaldosteronism. Can you help me out with this?
Sure! :D
The N’s are for sodium - Hypernatremia!
The C makes a K for potassium, which is less than the number of N’s, therefore, hypokalemia!
Also, Na+ is sodium. A could remind you of Aldosterone.
AL could remind you of ALkalosis.That’s all!
-IkaN
Post link
Does your pancreas need a boost? Our new insulin drop will give you a smile when you need it most.
Cute stylized insulin enamel pin features the amino acid chains that make up this peptide hormone, made in your pancreas.
Insulin is a hormone that helps turn food into energy. After you eat, sugar from food goes into the bloodstream. Insulin unlocks body cells so they can accept a special delivery of sugar (aka glucose). The cell transforms glucose into energy for you to run and play.
This is one of three NEW hormone pins (estrogenandtestosterone also in the mix) at iheartguts.com. check ‘em out or give our hormones a new home!
Post link