#ulcerative colitis
Yoga for Bloating, Digestion, Ulcerative Colitis, IBD & IBS
Try this gentle routine anytime you’re feeling bloated, gassy or your Ulcerative Colitis, IBD or IBS is flaring up. Just 12 minutes of mild movement for lots of relief. Can be repeated back-to-back if needed!
Subscribe for free weekly uploads: http://bit.ly/sarahbethyoga
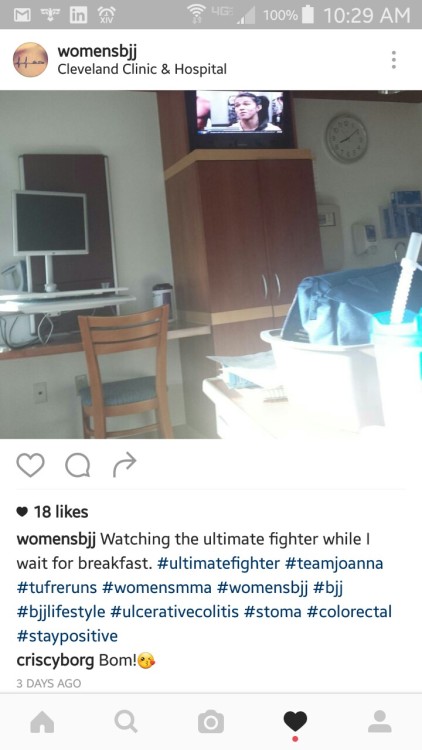
OMG omg, UFC fighter Cris Cyborg totally just commented on my photo! Totally made my day. I feel so legit right now!
Post link
I can atest. 1st surgery down 2 more to go before I can restart my journey as a white belt. Just need someone to send it back from the country I left it in! Lmao! Picture credit is all Meerkatsu!
Post link
Dr. said surgery was successful, still a lot of pain, but I should spend a week or few days here at the hospital then I’ll be ready to go home can’t wait to get back to my life of martial arts friends and family! In three weeks I can have pizza and I think walking is the only exercise but it’s better then nothing. #nocolonnoproblems
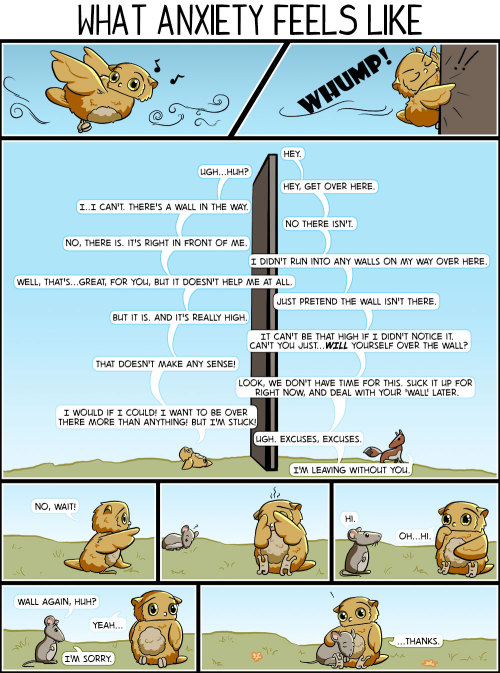
So I was kinda whiny and full of feels yesterday. I was also prepping for a colonoscopy that is happening in a few hours. (Hurray for chronic illnesses!) This meant I had to drink massive amounts of nasty stuff. And I couldn’t eat anything that isn’t essentially a clear liquid. Neither of these improved my mood, especially being unable to eat comforting things.
Today I will be better. I will come home afterwards, eat Chipotle, smoke some dope, eat some more Chipotle and some Mega Stuf Oreos (not just Double Stuf), and then talk to my friends and finish something long and more interesting for this tumbla.
Hello, I hope you are all well. Thank you for sticking with me despite my lack of consistent posts. I’m trying to keep with the alphabet theme because it’s more interesting, I think. It also gives my posts a bit more structure, rather than me just rambling.
Anyway, today I want to talk about diagnosis. Specifically, a new diagnosis.
As you should know (if you’ve been following me for a while but don’t worry if not), I have Inflammatory Bowel Disease and Primary Sclerosing Cholangitis, as well as a few other less impressive-sounding conditions. The IBD and PSC I mention specifically because there are thought to be links between them, mainly that patients with Ulcerative Colitis (the form of IBD I have) are more likely to develop PSC than those without UC. This is known as an extraintestinal manifestation which means that other conditions may develop because I have IBD.
Other extraintestinal manifestations include condition such as arthritis, skin conditions, inflammation of the eye, anaemia, problems with the kidneys, and osteoporosis. That last one is what I want to focus on today.
Just to clarify, I do not have osteoporosis. I do, however, have thinning in the base of my spine which they found recently in a bone density scan. This, I believe this is called osteopenia, but I’m not 100% sure as my GP didn’t put a name to it. Anyway, the thinning isn’t too serious, by the sounds of things, but they do want to start a form of treatment to stop it from developing into osteoporosis. My GP is consulting my GI as she doesn’t want to start anything that may aggravate my IBD. In the meantime, I am doing daily exercises that are designed for those with sciatica. This may or may not help but seeing as how I do get mild sciatic symptoms from time to time, I don’t think this will do any harm.
Speaking of exercises, I am still doing my knee exercises, as it doesn get stiff if I’ve not moved around for a while, and I’ve also added abdominal core exercises to my routine to strengthen my core. My goal is to do them all at least once daily so that I am as strong as I can be to return to work in two weeks. I am also trying to stick to a routine of getting up and going to bed at the same time each day (even the weekends) to regulate my sleep and get my fatigue under control.
Thank you for reading and I hope you are keeping safe and well. Until next time!
Firstly, let me just say sorry for not posting in a while. As the topic of this post suggests, I’ve been struggling recently with several thing. Today though, I’m going to be talking about brain fog.
Have you ever walked into a room and forgot why you did so? Or maybe you forgot what you were about to say mid-conversation? That’s relatively normal if it only happens occasionally, as it’s easy to get distracted. However, if this happens a lot, like on a daily or even hourly basis, then you’re probably suffering from brain fog.
There are many different reasons that someone may have brain fog, but for me, it’s just yet another side-effect of living with IBD. Because of my IBD, my diet is a little complicated. This can lead to deficiencies (like anaemia, for example), which can lead to fatigue which in turn, can cause brain fog.
Brain fog is like walking into a room and forgetting why. Only, it happens all. the. time. You forget what you’re doing, why and even if you were talking to somebody. I’ve found myself stopping mid-sentence and realising that I can’t remember what I was just saying seconds before. I’ve also found myself forgetting what I’m doing (often at work) which can lead to me not completing tasks or making mistakes.
Because this happens so often, I’ve had to develop ways of dealing with it. And by that, I mean I write down everything. If my manager at work, for example, tells me to do something or change a bit of written work (which we are required to do to show we understand how to use the equipment), I make sure to write them down. I also try to do tasks in order so I’m less likely to forget something. I will then check with my manager that there is nothing I have missed. This usually works when my fog isn’t too bad but when it becomes worse, I struggle to remember simple things like my symptoms (if I’m speaking to a doctor) or what happened early that day. This is when writing things down does very little and I have to really think hard to recall things. Unfortunately, I don’t have a solution for this so it can look like I’m just really forgetful. Which is why it’s so important to talk about these issues. One of the things that I’ve found can help is to explain to the person you are talking to that you are experiencing a bit of brain fog and that you may need to be told things more than once. This lets them know what to expect from you and, hopefully, not get frustrated with you if you forget something or need things repeated to you. Never be scared to ask someone to repeat or rephrase something they’ve said.
Also, side note; having a chronic illness doesn’t automatically mean you’ll suffer with brain fog, and you don’t need to have a chronic condition to experience brain fog either. Just because someone else’s fog is denser, doesn’t make your irrelevant.
Living with a chronic condition can be tough because you are dealing with it on a daily basis. What can make it even tougher is when no one really know what your condition is or how it affects you. You never truly understand until you get it yourself, right?
Maybe you have made a new friend or started a new job but none of your colleagues know about your condition and that’s fine, you’re comfortable with it like this. But then you have to rush to bathroom for the umpteenth time that morning or perhaps they see you taking your truckload of meds at lunch. And they start to ask questions. What do you do? Do you shrug it off and say it’s nothing? Or do you tell them about your condition, bringing awareness to them?
Now, just to be clear, no one is forcing you to tell your story to anyone. You are not obliged to tell everyone who asks about your health situation (or anything else for, that matter). Telling your friend or colleague that “it’s nothing” is a perfectly fine answer and they should respect that you don’t want to tell them and if they try to push the issue, they are in breach of your trust and are not owed anything (not that they were to begin with).
However, if you do choose to share your condition with them, you may find things are a little simpler to explain; for me, telling some of my colleagues that I have IBD (and a stoma) was somewhat unavoidable; I was having issues with my stoma that were affecting my ability to perform my daily tasks at work so a couple of my colleagues found out. Although I didn’t feel 100% comfortable about sharing such personal information with them as we had not known each other for very long, it did make my life a little easier from that point on; my colleagues who knew were more aware of what I was able to do (ie. lifting heavy things was a big no-no at the time) and I didn’t feel like I needed to explain myself if I was rushing to the bathroom or needing to sit down for a moment, having overdone it.
I know, it’s not our job to educate the ignorant but if someone asks, helping them to understand a condition that affects so many but is otherwise unknown to those who do not suffer with it will help raise awareness and may even make your life a little easier. It’s your choice though, please do not feel like you have to tell someone about your condition/s just because they asked. They do not have a right to that information, it is yours to volunteer if you see fit.
[Please note: this was originally posted in early June on my main blog page https://what-can-i-eat.com/2020/06/02/a-is-for-awareness/]
Disclaimer/Trigger Warning: I debated for a while whether I should post this as it is a bit raw, but I feel it’s important to share every aspect of living with this disease. Please feel free to skip this post if you’d rather not read it.
*******************************************************************************************
*******************************************************************************************
“You’re being admitted.”
Those words have been spoken so many times to so many people. No one likes being in the hospital and it can be a frightening experience. But what about when you’re being told it for the third, fourth, fifth, eight, tenth time? Time seems to stop, and your stomach feels like it’s just dropped out. And then the negative thoughts about never getting better start up all over again. And your brain is there reminding you of all the previous times you’ve been in this exact situation. And you know the doctors and nurses are just trying to help you feel better but you can’t help but feel some minor resentment towards them and you can’t take it so you burst into tears, just wishing you could wake up from this nightmare!
That’s medical PTSD.
Post-Traumatic Stress Disorder is real and can happen to anyone. It should be talked about and acknowledged, regardless of your experience. And for a lot of chronically ill people, it centres on their condition/s.
My trauma stems from having been admitted to hospital ten times in just under four years and from having tried seven different medication, none of which worked to get me into remission. It comes from having had four surgeries in three years, two of which were emergencies to save my life.
Despite the nurses being incredible and amazing, despite the doctor’s efforts to help me, I still fear going into hospital because I know what happens when I do. IV fluids are the first thing to go up, usually followed by either antibiotics or steroids. This is to stabilise me whilst they decide the next cause of action. They do x-rays and CT scans to make sure I’m not obstructed and that my bowel hasn’t twisted as both have happened in the past. And depending on what the outcome is, sometimes they’ll insert an NG tube to drain my stomach, or perhaps a drain for an abscess. Sometimes, this will take a long time and I end up with a PICC line in my upper arm so they can give me TPN in place of food.
And sure, I’ve come out alive and mostly unscathed. I’m breathing and still able to move and work and take care of myself because of (or perhaps in spite of) what I’ve been through. But that doesn’t make it any easier.
People tell me I’m brave, but bravery implies there was a choice. I didn’t choose. I wasn’t asked. On life’s questionnaire I didn’t tick the box labelled “chronic illness”. That was something that was thrust upon me without my consent.
What I’m trying to say is that for me at least, hospitals are a source of endless trauma and fear, and even going in for a simple blood test or check-up puts me on edge.
I suppose I should say something positive about how I’ve got my family beside me keeping me grounded through all this. But the truth is, not even they know the full extent of how badly this has affected me. I’ve sought out therapy before and I dare say I’ll seek it out again before long.
I’m sorry there’s no happy ending to this article but thank you for reading if you’ve made it this far. And please know that whatever you’re going through, you’re not alone. Please stay safe.
Just a quick update on my last post: Back in August last year, when I had my last surgery, a small collection of fluid gathered near my liver and I had a drain put in to try and get rid of it. As it is impossible to drain every last drop, a tiny amount was left to be absorbed by my body over time. It’s quite unusual for such a small amount to stick around for as long as it has, but it can happen (so of course it happened to me). This tiny abscess has also caused a minor infection and this is what the doctors think is the source of all that pain and discomfort. I was admitted to hospital a couple weeks ago for a grant total of two days so they could do an x-ray, CT scan and bloods. They started me on antibiotics when they found the abscess which I’ll be on for the next week of so. I’m expecting to have to come back in for another scan to make sure the abscess has gone or at least to have another blood test to check on my infection markers. For now, I am resting and taking my meds.
Anyway, I hope everyone is staying safe.
So, as we all know, there is a pandemic at the moment. As someone with a chronic illness (and as someone whose partner has active asthma), I am concerned. I don’t want to catch coronavirus and I certainly don’t want my partner catching it. If we did, it would be extremely serious for us both.
I work for the NHS and so am classified as a key worker (as is my partner). Where he can work from home, I can not. I am currently at home due to an IBD flare-up (which I’ll get into in a bit), but I will eventually need to go back to work. The thing is, even though my work’s Occupational Health has advised I stay away from patient interaction, my job is patient-facing, so I’m not sure what I’ll be able to do when I do go back. And on top of that, what if I pick up coronavirus on my way home or from an asymptomatic colleague? There’s not a lot I can do other than opt to self-isolate. This will have to be something I discuss with my manager when I return to work.
As for the flare-up, it started about three weeks ago. We had just got back from the Netherlands and I was starting to experience stomach cramps. I put this down to having tensed during the flights as I dislike flying, namely take-off and turbulence. I thought they’d go away after a bit but no, they kept getting worse. Two weeks ago, it got to a point where I was having to sit down because I would get nauseous if I was stood for too long. That’s when the fatigue began to set in, to a point that my colleagues were starting to notice. They would tell me that I didn’t look well and that I should go home. I didn’t want to. The fact is, I haven’t been at this job for a year yet and my probation period had already been extended due to two instances of sickness (both of which I was hospitalised). If I called in sick, that would be three instances within the first nine months of my employment and I didn’t want to risk losing my job (despite all the reassurances from my colleagues to the contrary).
Come Friday of that week, and I am feeling awful. Thankfully, Friday afternoons are quiet for me at work so I didn’t have to do a lot. I decided I would use the weekend to rest and evaluate my condition Monday morning. I think they saw it coming as my manager was not surprised when I called in. I was signed off for two weeks. That two weeks is almost up and, unfortunately, I am not feeling much better. If anything, the pain is worse. I’ll be speaking to my GP again Monday to extend my sick note. It sucks but I have been advised by my GI to stay at home if I am experiencing flare symptoms. Hopefully, things will settle down soon and I’ll feel well enough to return to work.
Anyway, to everyone who reads this, whether you have a chronic illness or not, stay safe.
I know I’m a little late, but here is what happened when I flew to Amsterdam a couple of weeks ago.
At our local airport, they have a metal detector and, more recently, a body scanner. This scanner is designed to detect anything that might be hidden under clothing, such as a weapon or other items. This included my ostomy. I can’t say I was surprised by this as it has been picked up before when we last flew. The security guard was polite and, after scanning under my hood with a handheld scanner, she asked if I had anything on my stomach. I explained I had an ostomy and, to my surprise, she smiled and took me to a side room, along with another female colleague. She said she didn’t need to see my bag but didn’t want to scan it in front of people and chose to do so in the side room as this gave me more privacy. It took less than five minutes and they were both very polite and kind about the whole thing. They wished me a safe journey and that was that.
I have read some of the horror stories other ostomates have shared about their experiences when going through airport security (one had been asked to open their bag, another had their bag ripped off their stomach without their permission, ect). Needless to say, I was a little nervous, despite our previous time flying having been without incident.
Thankfully, I was able to put my mine at ease before even arriving at the airport by visiting their website. My local airport has a “special assistance” section which included a helpful “tips” pdf. Reading through, I found that not only were they part of the green lanyard scheme (which helps staff identify passengers who have a hidden (or not so hidden) disability or illness), but they have also done a load of training with a list of charities, including Stomaware and Crohn’s & Colitis UK. This means that their security are aware of sensitive subjects like IBD or a stoma, and know how to proceed without invading someone privacy or dignity. All in all, I was quite impressed with how they handled things.
Now, I don’t know if any of you have had to squeeze into the on-board toilet, but from previous experience, I didn’t want to have to go anywhere near our planes facilities, especially with my bag; the cubicle is tiny and I know output can be smelly and I didn’t want to be the one to stink out the entire plane. Thus, I decided I wasn’t going to use it. But how was I going to ensure my bag didn’t fill up whilst in the air? Simple; I took extra loperamide throughout the day and before boarding. I also made sure to eat a small, carb-filled meal (we were flying around dinner time) and a bag of jelly sweets. Thankfully, this worked. I would like to point out that this only worked for me because my output is usually quite watery. If it were ostomy-normal consistency, then I probably wouldn’t have needed to do any of this as the flight was only about an hour.
Conclusion: flying with an ostomy is way easier than I thought.
I would recommend anyone who is planning on flying with a medical appliance seek advice from your airline provided/airport. It can’t hurt to let them know before boarding.
Although not always necessary, a travel certificate might help if you are taking a lot of supplies with you. And if you are taking medication, always keep it in the original packaging. One last thing, put your medical supplies in your hand luggage. You don’t want them getting damaged or lost whilst in the hold.
For a while now I have been having palpitations on and off for no particular reason. I started checking my heart rate, using a built-in app on my phone, on a somewhat daily basis shortly after my IBD diagnosis back in 2016 and noticed my resting heart rate was always above what the app said was normal for someone of my age/height/weight/gender. I didn’t think much of it because I was on a lot of meds that, for all I knew, could be causing the increase in heart rate. It was always high whenever I was admitted to the hospital too but I assumed that was due to being in hospital as well as being unwell at the time.
Skip forward to just after my first surgery, and my resting heart rate was always above 120bpm. For reference, for an average adult of my height/weight/age/gender, the resting heart rate is typically between 60 & 80bpm. I figured the 120bpm was a direct result of my surgery and after a few weeks of slowly building my weight back up, my resting heart rate dropped to around 90bpm or so.
From there, I didn’t really notice it much; it became sort of like background noise. I’d notice my heart beating really fast during and after exercise but didn’t really think much of it then either because that’s meant to happen, right?
Anyway, after having surgery for the fourth time back in July last year, I started getting sudden onset palpitations with fast breathing and a somewhat panicked feeling (a panic attack?). Again, for no apparent reason. This would last for about 2 minutes before fading, leaving me feeling drained and anxious, so I finally went to my GP. She referred me to have a 24 hour monitor, which involves wearing a heart monitor (similar to an ECG) for 24 hours that records the wearers heart rate which is then analysed by a cardiologist.
After having the 24 hour test at the beginning of the year, I finally saw a cardiologist in clinic earlier this week. They did an ECG and an ultrasound on my heart and, thankfully, everything looks normal. My heart infrastructure is fine and looks healthy, and aside from the palpitations and high resting heart rate, there doesn’t appear to be anything wrong. They don’t want to try any intense treatment unless it starts interfering with my daily life but they did recommend trying beta-blockers to help regulate my heart rate. Because beta blockers can make you tired, the cardiologist said I wouldn’t have to take them all the time but could try taking them whenever I start getting palpitations.
My GP has already filled a prescription for me so I guess I’ll give them a go once they’re ready. Whether this is related to my IBD or not, I don’t know, but it wouldn’t be too much of a stretch to think so as IBD can effect many parts of the body, not just the bowel. I’ll update again on this after I’ve been taking the beta blockers for a bit.
In other news, I’m going to flying to the Netherlands later this week so expect a post about that later next week. I’ll be sure to take note of how going through security goes this time compared to last time (hopefully, it’ll go just as smoothly).
I saw my GP this morning regarding both my loperamide prescription (I’ve been having a reaction to the liquid so needed a new script for the instand melt tablets) and my rehydration methods. She said she was happy to do a monthly prescription for 112 instant melt tablets of loperamide and I can always adjust the dose as I need to. So that’s one thing fixed relatively easilly.
When talking about my rehydration, she admitted she wasn’t as knowledgable about it so she would email my dietitian for me. I explained my reasons for no longer having the St Mark’s rehydration solution and that I was instead drinking Lucozade and a suppliment drink called Sneak as both have a somewhat decent amount of sodium/salt.*
As I had a blood test just yesterday (Thurday) morning, she had a look at the results and it showed that my sodium was back to normal levels as were pretty much everything else. I asked if I should keep going with what I am doing and she agreed. She said she was still going to email my dietitian just to keep them in the loop which I am more than happy for her to do.
All in all, A good visit to the doctor. I just need to wait for my loperamide to be ready.
*Just a quick disclaimer: I am drinking Lucozade and Sneak suppliment drinks as a replacement for the St Mark’s rehydration solution as this works better for me personally. Please do not change or stop your rehydration methods recommended by you specialist/GP/dietitian without talking to them about it in detail first. Be safe.
It’s been a little while since I last updated but there hasn’t been a lot to share. Seeing how it’s Christmas though - and we all know how fun that can be when it comes to the eating part - I thought I’d write a little update of how things have been since last time.
So, having since seen the dietitian and tried (and failed) to eat more fruit, I have started taking a multivitamin daily and have been having the occasional fruit smoothie (usually consisting of a bunch of bananas that are near going off and some chocolate chips and/or honey). I still have some tinned fruit which I’m planning of turning into smoothies at some point. Other than that though, I have been avoiding having much in the way of fruit and veg because of how badly my attempts to eat even just a little bit have gone. My stoma nurse agrees that I should listen to my body and eat what I know is safe for me, feeding back to my dietitian when I next see her.
As for the low sodium, I’ve given up drinking the St. Mark’s rehydration solution because it makes me super thirsty and I always go over my 2 litre daily fluid limit. Instead, I’ve been having other drinks like Lucozade and Sneak supplement drinks as they contain sodium as well as a load of other extra vitamins. With these, I’m able to stay within my daily fluid limit and I don’t feel thirsty at all by the evening. I realise this isn’t the same as taking the St. Mark’s solution, but it works better for me, and I am going to speak to my GP in the new year to make sure she is happy with what I am doing.
On a more positive note (minor TMI warning), I was able to eat Christmas dinner (complete with a few veggies) and so far so good; I haven’t had any issue passing anything and my stoma output has been ideal, with only a tiny bit of pancaking but no leaks! I was able to have carrots, roast potatoes as well as a spoonful of mashed swede, a piece of cauliflower and a single parsnip. I want to try and add more veg to my weekly meals, even if it’s just some carrots and potatoes, so this is a positive sign.
Anyway, whatever you celebreate, I hope you have had a fun-filled and safe 25th December.
I saw the dietitian early last week and it turns out my sodium is super low. She recommended I start drinking 1 litre of the St Mark’s rehydration solution daily and 1 litre of other free fluids. She also said I need to start reintroducing fruit and veg and gave me some info on how best to do so. She recommended tinned fruit as a good alternative to fresh fruit as it’s softer and has already skinned, so I bought some tinned fruit to try.
A few days after seeing her, I tried having a few bits of tinned apple and mango. It went through me fine but my output for that afternoon was near solid so it ended up pancaking in the bag and almost caused a leak at work. Thankfully, I had my emergency kit with me so I could change in the toilet. I left it another couple of days before trying the apple again (leaving out the mango because I thought this was a bit too physically fiberous for me), but once again, I pancaked and had to change at work. Since then, I’ve stuck to banana’s and smoothies because I don’t want to risk another leak, especially if I’m not at home. I’m also going to start taking mutlivitimans daily and try to have fruit smoothies more often. I know I can eat carrots and potatoes when they are peeled and cooked well so I’ll be doing that too.
I know the fruit didn’t cause a blockage but it could have done and I’m so scared of being hospitalised again. I feel as a medically trained dietitian who’s working with new and veteran ostomates, she should know more about how certain foods effect the stoma output as well as the intestines. If I was brand new to having a stoma, I’d have followed her advise and probably be dealing with leaks if not a full-on blockage. I’ll be sure to let her know of the outcome of her advise when I see again early next year. (Don’t worry, I’ll be nice.)
I saw my GI a few days ago, and I was expecting to only see him. To my surprise, I actually had a joint GI/Liver appointment. This is really helpful for them and for me as having IBD, and Ulcerative Colitis specifically, means I am more prone to certain liver diseases, and seeing me at the same time makes it easier to assess and treat my symptoms without having to keep going back and forth.
Just over a year ago, I had some problems with my liver. An ultrasound showed it was enlarged after I presented with abdominal pains to A&E, and I had a biopsy to determine if I had something called Primary Scleroring Cholangitis (PSC), a progressive autoimmune disease that causes the bile ducts in the liver to become inflammed and eventually blocked. At the time, I didn’t think I had this as the biopsy didn’t show any signs of it - or so I thought. As it turns out, I do have PSC but it is very very mild at the moment. It means I’ll need yearly ultrasounds but that’s it unless it shows signs of progressing, then I’ll need biopsies. At the moment, there are no treatments for PSC but it is something they are working on.
As for my IBD, everything is fine. My GI wants to check my sodium and calprotectin so I’ll be doing several samples and blood tests over the next few months. In the meantime, I’ve been advised to have St. Mark’s rehydration solution or dioralyte every now and then or if I’m feeling very thirsty during the day. This should help keep my electrolytes up and save me from getting dehydrated.
I love Halloween. I love it for the decorations, the costumes, but most of all, I love it for the sweets. Yes, the sweets. (I know, I’m a big kid really). But seriously, there is a practical reason for my eating many sweets; slowing down stoma output without having to take medication.
Recently, I have had fairly loose output which is a bit of a pain because it can mean the bag filling faster than normal. Eating sweets, particularly ones with gelatin in, can help thicken the output and slow it down. Halloween is a great time to stock up because not only is there a much higher supply in shops, but they can be a bit cheaper. Now, obviously, I’m not saying everyone should gourge themselves on sweets (I’m no doctor but I’m pretty sure that’s not good for you, even for ostomates) but this is just how I like to deal with high and loose output. How do you deal with loose output?
So, my plan for tonight are to eat Chinese take away followed by a load of sweets whilst watching Coraline. What are you up to this Halloween?
I went to a Crohn’s & Colitis UK coffee morning today with my mum. It was good to meet new people, we talked a lot but there’s never enough time to speak to everyone. I hope to go to the next one near me though. I met someone who has had a jpouch for around ten years now, and I spoke to someone who came with their mum (like me) and who both have Crohn’s. A couple of them were also at the IBD open day last weekend too. I’ve always thought that these meet-ups are a good idea, they give you somewhere to talk freely and feel safe, as well as being part of a community that understands and doesn’t judge because they’ve been there. I know they’re not for everyone but I enjoy it.
In other news, I saw my surgeon last week and he’s very happy with how I’m doing. He said he doesn’t want to do anything now for at least another year, which is fine by me (two surgeries is more than enough for this year, thank you very much). He said I’ve got three options though; 1) I can have my stoma closed and try the jpouch again, 2) I can have my jpouch & rectum removed, a permanent end ileostomy formed and have a barbie-butt, or, 3) I can stay as I am with jpouch & rectum intact and loop-ileostomy. I am quite content to stay as I am for now, but eventually, I will want to go for option 2; permanent stoma and barbie-butt. I don’t want to go back to the jpouch because not only is it ulcerated, but I still have the perforation near the entrance, both of which make me not want to risk it failing again and having to have yet another surgery. I could stay as I am indefinitely but I think I’ll always feel like it’s not finished and I just want this to be sorted once and for all.
So, that’s it for now. Work is going well and I feel able to do more things and for longer. My appetite has returned with avengence so I’m eating like a horse at the moment. My weight is very slowly increasing so all good from where I’m sitting.
I went to an IBD information open day today at my local hospital. There were lots of resources for patients as well as their friends and family, and the talks covered things like exercise, research, diet and the hospital’s IBD helpline. Even though I know a lot about my disease already, I still found it informative and interesting. There wasn’t much time for networking or socialising but it was still good to be there among those who suffer as well and those who are helping make it bearable.
Next week, I’m going to a Crohn’s & Colitis UK coffee morning meet up. I haven’t been to one for a while so I’m looking forward to seeing how everyone is doing. Although I don’t feel I “know” any of the regulars at the meet-ups, I still feel some sort of connection because we have this disease in common.
As for how I am doing, I feel my recovery is going well. I went back to work three weeks ago and it’s going well so far; I’ve a gradual return, with my first week consisting of one and a half weeks because I had a week of annual leave straight after. The second week was two full days but they were easy as it was quiet and there wasn’t as much to do. This last week I worked four days with a day off in the middle to give me time to rest. I have found getting back into it easier than I thought and there are only a couple of minor adjustments I need at the moment. These adjustments are mostly regarding my ability to aid a disabled patient, specifically mobility aid users, as I can’t push a wheelchair nor support another person due to my stomach muscles still healing. This is to protect both me as well as the patient as if I am unable to support someone and they fall, I can’t help them back up again. It’s frustrating because I hate how I am not able to help my patients the way I should. Still, this is only temporary for me and I know eventually I will get better. I am for the forseeable future going to keep wearing my support belt as it helps prevent muscle pains during my work day.
As for my diet, it’s great; consisting of lots of bread, crisps, chicken, potato and chocolate. I’m not underweight but I’m on the lower end for my height so it wouldn’t hurt for me to put some back on. Plus, I’m almost always hungry so snacking is a good thing as far as I’m conscerned. This need to snack does pose a slight issue with my work though as I only get one break during the day and, no, unfortunately I can’t split it due to task assignment. I may have to start stashing snacks in various places so I can eat when it’s quiet.
Anyway, that’s all for now. Hopefully, I’ll have more to share over winter with the cold weathers effects on stoma bags etc, as well as the perils of Christmas dinner. Thank you for reading!
Why am I using my stick today when I didn’t need it yesterday?
I am travelling by train for the first time since my surgery. The journey involves several changes and I am carrying quite a full backpack. As I am still recovering, I need to be careful that I do not fall or get knocked into as these could both potentially cause muscle strain that can lead to other complications. Although I haven’t needed my walking stick for the last couple of weeks, having returned to work this week has shown me that I am far from fully recovered.
As my work requires me to be on my feet a lot, by mid-afternoon yesterday my stomach muscles were beginning to protest. I thought this ache would go away if I sat down and hugged my hot water bottle when I got home but, unfortunately, the pain persisted throughout the night and I am still quite sore even now.
What does all this have to do with my using my walking stick today? Well, as I am travelling through the busy London underground for part of my journey, it will not only help support me as I walk around, but it will also act as a “red flag” to other commuters that I won’t be able to move out of their way and to be mindful to not jostle me as they rush for the tube.
I have said this before but I think it’s worth repeating because not everyone understands that you can be fine one day and not the next. Recovery is not linear.
I saw my stoma nurse earlier this week and, after a brief chat, we decided I may need a convex bag again but because she was conscerned my stoma might prolapse if the bag was putting too much pressure on my bowel, she offered the Salts 1-piece drainable convex bag to try for a bit as they are meant to be more flexible than other convex bags and so shouldn’t put as much pressure on the bowel.
It’s a tad bit smaller than the Sensura Mio, with a petal shaped baseplate and a drainage end similar to the Dansac drainable, except it has a small tab on the end which makes opening it easier. The material used to cover the bag is soft, water repellent and makes the bag look a lot less clinical. First impressions after wearing it for an afternoon where that it was a good bag that held it’s shape fairly well when full and that didn’t rustle when moving.
But.
I had issues with the opening. I found, although easier to open and clean than the Dansac, it was still messy and would leak a tiny amount of output when closed because it lacked the extra side tabs that the Sensura Mio has.
I thought that maybe I could get used to the opening but then I realised that I was scratching myself raw around the edges of the baseplate - something I was told shouldn’t happen because there is aloe vera in the adhesive to prevent such itchiness. If this was the only issue then I might not have minded too much but because of the opening as well, I’ve decided I prefer the Sensura Mio.
That’s not all to say that the Salts bag isn’t any good. I like it, I really do. It’s just that I can’t get on with the opening (I guess the Sensuro Mio has spoiled me?) and the reaction to the adhesive. I don’t want to deal with the tiny leaks or the itchiness, things that I haven’t had with the Sensura Mio.
I have had other ostomates mention/recommend other bags to me so I may try them in the future but, for now at least, I’m happy with what I’ve got.
I have had four surgeries on my gut in the last two years. As you might imagine, this puts a lot of strain on by stomach muscles. Muscles we use for pretty much everything, from carrying to simply standing.
When you first start moving after surgery, every twist, every step is painful and you feel like you might just rip your stitches open at any moment. Thankfully, while in hospital, there is always someone to help you, to hold your arm or fetch a wheelchair for you when you can’t quite make it back to your bed. However, when you’re home and out in the real world, those safety nets are always there.
It takes a while for your muscles, and in fact your whole body, to recover and adjust to how things are post-surgery. Sure, a friend or family member will likely be with you on every excursion out the house for the first few weeks but what about when you want to go out when no one can go with you? What about even when someone is with you but you’re not sure you’ll make it to the car, let along the cafe you’re going to for lunch?
That’s where mobility aids come in.
I have a walking stick. I am 31 years old and look fairly healthy, albeit a bit skinny, and I have a walking stick. I got it for the very reasons mentioned above. I can go out with family, sure, but they can’t always hold me and most probably couldn’t lift me if I fell. The walking stick acts as a support for me if I stumble or when going up or down steps, it allows me to keep my independence. It allows me to walk further and for longer and gives me the confidence to go out on my own.
But it’s not only that. It also acts as a warning to others who can’t see the scars, the ostomy bag and the healing wounds, that I may be slower, unable to move out of their way or cross the road in time. It lets people know to give me a little extra space, to catch that door or hold the lift.
My point is that mobility aids are useful and we shouldn’t be ashamed to use them just because we may look healthy or young or otherwise as if we don’t need it. If you feel you need a mobility aid, regardless if it’s a wheelchair, a walker or a walking stick, you should use it. It doesn’t matter if it’s for six days or for the rest of your life, you should use the tools at your disposal if it makes life easier for you.
And to anyone who has felt the need to question why someone is using a mobility aid, it’s none of your business. You don’t know what’s going on inside, what that person is dealing with. They may be walking fine but that’s probably because they are using that mobility aid. Please don’t be so quick to judge.
Nurse: Is it okay if I do a quick rectal examination?
Me: *already pulling pants down* Do what ya gotta do!
Nurse: I’m so sorry, I know this is really unpleasant.
I’m a veteran, trust me. I’m so desensitized to this sort of stuff.