#crohns
Family doc and GI down, Gyno to go tomorrow.
I’m not anticipating any more follow up at the gyno, so I figured I’d post about updates now.
My GI appointment was actually pretty interesting. I mentioned the weird issues I’ve been having with perianal symptoms (itching, discomfort, pain while pooping, some really minor bleeding, and being awoken at night due to itching), and she did an exam to check for fistulae. She didn’t see anything, but did say that they can be pinhole-sized, so she ordered an MRI to check and make sure there’s nothing there.
Due to my increased frequency, the fatigue, and general malaise I’ve been experiencing lately, I’m also getting scoped at the beginning of August. She palpated my belly, and asked a few times if it hurt on my lower right (not more than usual), so she may be feeling something there that I’ve just not noticed, or have gotten used to. I mentioned that we will be trying to get pregnant within the next few months, so she said that any investigation should be done now. We can make sure everything looks good to give me peace of mind before trying, and if there are issues, we’ll deal with them. Increasing Humira, or switching to Entyvio or Stelara were mentioned.
I’ve done a round of normal bloods, but she also ordered the antibody test for Humira - Anti Adalimumab. Apparently a nurse will come to my home to do this. Hopefully, I can get it arranged for this week, before I inject on Sunday. Otherwise, I think I’ll have to wait until a few days before the injection following this next one.
Just waiting on results and test dates now. Anxious to see how everything looks.
Hey everyone! I’ve not been updating as much lately because there hasn’t been a whole lot that’s new.
Last weekend, I did my second Gutsy Walk for Crohn’s and Colitis Canada! I again made it to Top Pledge Earner status thanks to my generous friends and family, so I guess that’s gonna be my benchmark every year
This week and next, I have three appointments. I saw my family doctor today for a skin check, and he doesn’t like the look of a new mole that popped up on my fourth toe (of all places), so I’m being referred to a dermatologist to likely have it excised. Kinda scary, but I’d also rather be safe about it. So, I guess I’m now adding dermatologist to my collection of doctors, ha ha! (Seriously, I have a GP, GI, rheumatologist, ENT, gynaecological oncologist, endodontist, and I’ve also seen an infectious disease specialist in the past )
Next up is my GI on Thursday, and there’s going to be a lot to discuss. As mentioned, I’m not confident that humira is still as effective as in the past, and I’ve had some odd things going on. The random hive issue, perianal problems, and hair loss that’s returned. I’ve also had major fatigue for the past month, and increased frequency. I’m sure there will be labs ordered, and probably a scope as well. My husband and I are also (we think) FINALLY going to start TTC in the next few months. I want to make sure I have my ducks in a row before we start the process.
Monday next week I have what is hopefully my last repeat pap after my abnormal result and the colposcopy that followed. If it’s all clear, I’m good to go for only having annual paps again! Yay!
So much happening, I’m tired just thinking about it.
Hey Crohnies, if anyone out there has tried and failed Humira, could you let me know what failure was like for you?
I’m starting to suspect that it is losing effectiveness.
Lately my frequency has increased from 1-2 times a day to an average of 3-4. Slightly increased pain, and massive fatigue. I’m sleeping a minimum of 8 hours a night, but I’m dragging myself out of bed, falling asleep at work, and needing naps. Feeling some general malaise.
I’ve had two instances of a random hive popping up on my stomach (I’ve never had hives before, anywhere), for seemingly no reason.
I’m also losing hair again
I have a GI appointment in June, and I’m 99% sure I’ll need a scope to investigate. It’s also been over a year since my last one, so I don’t think I’m escaping this time. I’m going to mention all of this to her, and see what happens, but I would appreciate opinions!
Getting quite concerned that I’m entering flare-time.
Not acceptable.
My excision is scheduled for September 11.
I spoke with my GI last week about what’s going to happen next. For right now, she has stopped Humira until we see what the surgeon has to say. She also has the pathology report, but I haven’t asked for, or gotten any details about the type of melanoma, or the possible staging.
Apparently any kind of aggressive cancer regardless of stage is not a good combo with the immune suppression of Humira (of course), hence the stoppage. If I have breakthrough symptoms, she mentioned prednisone (). Depending on what the surgeon says, and whether I have any other spots on my body that are suspicious, we may switch to Entyvio to be safer given it’s gut-targeting, rather than whole-body effects.
Given all of the side effects and complications I’ve experienced thus far, I can’t say I’m a huge fan of Humira. But, it’s gotten me into remission, and my symptoms are well under control. I’ve never been hospitalized due to my disease, and have not needed surgery. I’m so lucky that this drug worked for me.
As it stands, I’ll miss three full doses of Humira before the excision, and possibly more afterwards. I did ask about getting an earlier appointment to reduce the time off the drug (and the horrible waiting in limbo), and they offered me one this coming Wednesday. Maybe this is stupid, but with Wednesday being the day before my in-laws arrive from overseas, and the start our long-awaited holidays, I opted to wait until the originally-scheduled time. We’re going to be busy doing all kinds of activities: hiking, walking, touring around, and lots of driving.
I don’t know what this excision will involve (skin graft/amputation is possible), or how mobile I will be given the position on my toe. Just the biopsy was quite a lot more painful than I was expecting. I don’t want to ruin my holidays and everyone else’s as well, especially when the surgeon didn’t seem to think it needed to be done on an absolutely urgent basis.
To make this decision look less ridiculous, I’ll just say that I did ask my GI to let me know if she thought I should take the earlier appointment. She has the path report, and would hopefully know what we’re dealing with. She didn’t return my call, but her secretary confirmed she was aware of the question, so that makes me feel better. If she had told me to get in ASAP, I would have done that without hesitation.
Now I just have to wait and keep an eye on Crohn’s symptoms. I’ve had some increased frequency which I’m sure is due to stress, but nothing to be too concerned about yet. My GI told me that my scope showed deep remission, so I’m just hoping that I can hold on to that without Humira, and that I won’t have developed resistance to it when I get back on.
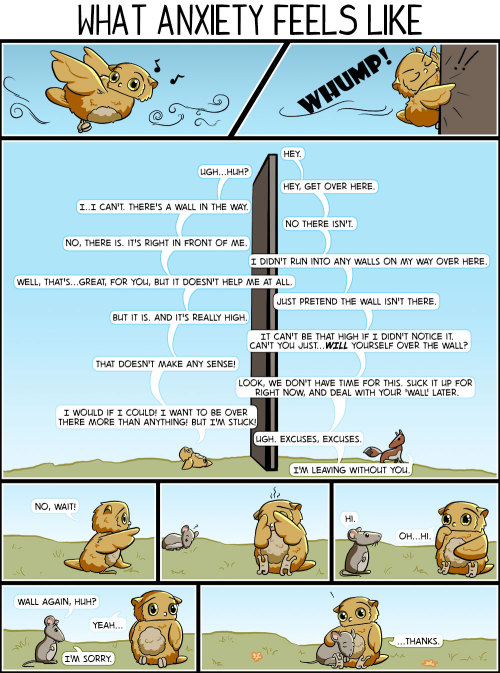
Anyone with a similar experience, please don’t hesitate to send me a message. Whether you have Crohn’s and melanoma, or just melanoma, or for that matter, have ever had a surgical excision on a toe, a tiny bit of insight into what I can expect would really help with my anxiety over this.
I’m already researching prenatal vitamins to start taking asap.
So excited!
Prep is going as well as can be, and it looks like it’s almost at the optimal level of effectiveness already.
One more sachet of pico salax tomorrow morning at 5:30, and then I’m off to the hospital at 10:15.
Please wish me luck. I’m actually quite nervous about this one because if the scope doesn’t look great, I will likely have to delay trying for a baby even more. I’m not sure how it will look in there, given the symptoms I’m having.
Interesting. Having some fairly significant lower-right quadrant pain today. Usually mine comes and goes but this has been at about a constant 4ish and approaching 5 at times.
Scope can’t come soon enough.
I’ve been feeling nauseous after eating since last Thursday. Also having lots of acid reflux, and it woke me up the other night.
On Saturday, I felt so unwell while waiting for Canada Day fireworks. My husband actually suggested that we go home, cause I felt and looked like hot garbage. By the time we came home (stuck it out because Canada), I had chills and a 100° fever.
I’ve had no fever since then, but last night the intense nausea struck again after dinner, and I had to take gravol and go to bed. The gravol actually didn’t help much, and I was up a few times feeling like I was on the verge of vomiting, but nothing actually came up.
So far today I’ve had a breakfast pita thing, and soup, and I feel reasonable. Going to try bland dinner and see what happens.
I have no idea if this is Crohn’s or some kind of bug?
I never know what’s happening with my body because my symptoms never seem to be the same. First flare was 12+ bloody diarrhea bathroom trips, pain, fatigue, and weight loss. Flare #2 involved joint pain, pain around my terminal ileum, but no blood, and not much diarrhea. Whatever the eff this is has so far included: perianal symptoms, nausea, fatigue, general malaise, and some pain around my terminal ileum (but nothing severe).
Do not know what to think.
Last week, I saw an Instagram story that made me pretty mad.
This particular person is vegan. Fine. I admire vegans for their dedication, and think it can be an extremely healthy way to live (if eating a balanced vegan diet, of course).
The thing is, it’s not healthy for everyone. Particularly, some people with IBD who can’t tolerate a vegan diet.
This is not to mention the whole concept of choice. Some people choose to be omnivorous, or vegetarian, or vegan, or fruitarian, because that diet is better for them, and there should be no shaming of anyone for the diet they choose to follow. Unless that diet involves cannibalism. That is not ok (obviously).
Anyway, back to this post. The poster was telling people to go vegan, and watch a new documentary about veganism and health on Netflix. Fine.
The next part of the Instagram story featured the following: “A plant based diet can help/treat the following: diabetes, heart disease, Multiple Sclerosis, Prostate Cancer, arthritis, Chronic Fatigue, and Crohn’s/UC.”
Ok. Ignoring all the other conditions listed (because I’m not a patient and can’t speak from experience, but seriously?), for Crohn’s, just no.
There is no diet that treats or cures Crohn’s, and the ignorance around food and this disease drives me nuts.
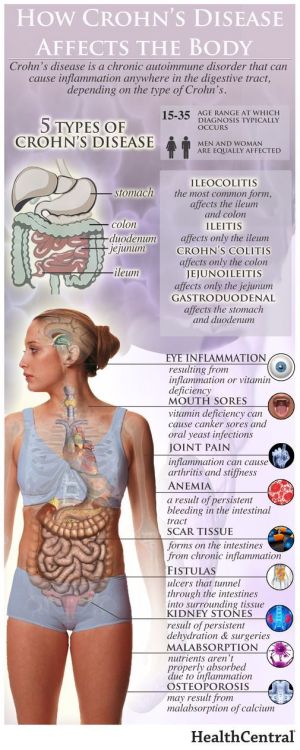
We do not know the cause of Crohn’s Disease. Do environmental factors play a role? Very probably. Is there also a genetic component? Yep. Can you modify diet to try and soothe an inflamed digestive tract? Yes. Is there any evidence that dietary change will cure the disease? No.
It is autoimmune and there is no cure
Stop shaming IBD patients for our disease
For so many Crohn’s sufferers, major components of a vegan diet are just not possible. When I’m sick (and frequently when I’m not even flaring), I can’t tolerate fibre. No leafy greens, vegetables of any kind have to be cooked to mush (and even then, cause pain), nothing with any kind of skin or rind, no nuts, no beans/legumes or pulses. Even whole grains are a no go.
I can basically eat bananas, potatoes, rice, plain chicken, white bread, dairy (I know, I’m weird), and high fat/sugar things like pudding or jello.
For others with Crohn’s, veganism is achievable, and that is truly amazing. The fact is that it’s not for everyone, and I find it highly offensive to suggest that just by going “plant based” and “loving animals enough to not eat them/their products,” that someone who is currently pooping blood 20 times a day no matter what they eat, or someone on TPN, can just heal themselves.
This whole concept of “if you would just do this simple thing, you can help yourself,” is obnoxious, ignorant, and offensive. Especially when it’s prescribed for everyone regardless or circumstance.
It suggests that our GIs don’t know what they’re doing by prescribing the best possible medical/surgical treatment options for us.
It also suggests that we are to blame for being ill.
That is not friendly or loving. Let’s just stop policing the food choices of others, and call it a day.
Pretty sure I need contrast. Let ya’ll know how THAT goes

Welp, that last post about not anticipating any gyno follow up really bit me in the ass
I was supposed to be having the second of my 6-month follow up Pap smears today. That’s not how it turned out.
My doctor was joking with me that this would be one of the last times I’d be looking at my cervix, and did the smear swab. Then he sprayed with the vinegar solution, and obviously noticed something he didn’t like the look of. He told me he’d be taking a biopsy. While this was a lot better than the first colposcopy I had, it still hurt like a bitch.
Then he said he wanted to do a scraping of the inside of my cervix, in the area he couldn’t see with the colposcope. “Some cramping” ensued, and there was a pretty decent amount of bleeding, so he had to use whatever that peanut butter-looking coagulant stuff is. Unpleasant.
That second scrape made me really nervous because he hasn’t done it before. I’m not sure why he thought it would be needed now, but hopefully he’s just being thorough.
He didn’t book a follow up right away, which makes me feel slightly better, but said he would call with biopsy results in a few weeks.
I asked him about TTC, and he advised me to wait. He said that it would be safer to make sure the biopsy is negative (of course) first, but that if I get pregnant, they can still do some treatment if needed. Usually changes take a long time to develop/worsen, apparently.
So, that’s awesome. Just waiting with baited breath now!
In other news, my last poke/prod of the week is scheduled for Friday when the Humira nurse is coming to my work to do the blood draw for the antibody test.
My joints ache and I’m tried all the time and it’s times like these where I hate having a chronic illness
julian-is-vibing-here-deactivat:
anyone know any good apps for keeping track specifically of food and symptoms? i wanna see if i can figure out some trigger foods (beyond the obvious stuff like hamburgers and smoothies that’ll send me into a flareup within like five minutes of eating them)
Personally I haven’t found an app that I really like but since I’m a total geek when it comes to data and computing, I love spreadsheets and databases for organizing and tracking things. Airtable in particular is excellent because it’s user friendly and is pretty to look at (mobile app or just airtable.com)
Plus organizing your data in this manner makes for endless possibilities.
As an example, right now I can only eat pureed food so this is a table I’m using to keep track of ingredients my stomach can tolerate to make smoothies:
https://airtable.com/shrH3T1bjZvWTm4Bd
You can export it as a pdf or csv for sharing, or you can use it to make easy to fill out forms! Example:
https://airtable.com/shr2P5KrBN5snrB8i
Hopefully you or someone else can love using this as much as I do
For a while now I have been having palpitations on and off for no particular reason. I started checking my heart rate, using a built-in app on my phone, on a somewhat daily basis shortly after my IBD diagnosis back in 2016 and noticed my resting heart rate was always above what the app said was normal for someone of my age/height/weight/gender. I didn’t think much of it because I was on a lot of meds that, for all I knew, could be causing the increase in heart rate. It was always high whenever I was admitted to the hospital too but I assumed that was due to being in hospital as well as being unwell at the time.
Skip forward to just after my first surgery, and my resting heart rate was always above 120bpm. For reference, for an average adult of my height/weight/age/gender, the resting heart rate is typically between 60 & 80bpm. I figured the 120bpm was a direct result of my surgery and after a few weeks of slowly building my weight back up, my resting heart rate dropped to around 90bpm or so.
From there, I didn’t really notice it much; it became sort of like background noise. I’d notice my heart beating really fast during and after exercise but didn’t really think much of it then either because that’s meant to happen, right?
Anyway, after having surgery for the fourth time back in July last year, I started getting sudden onset palpitations with fast breathing and a somewhat panicked feeling (a panic attack?). Again, for no apparent reason. This would last for about 2 minutes before fading, leaving me feeling drained and anxious, so I finally went to my GP. She referred me to have a 24 hour monitor, which involves wearing a heart monitor (similar to an ECG) for 24 hours that records the wearers heart rate which is then analysed by a cardiologist.
After having the 24 hour test at the beginning of the year, I finally saw a cardiologist in clinic earlier this week. They did an ECG and an ultrasound on my heart and, thankfully, everything looks normal. My heart infrastructure is fine and looks healthy, and aside from the palpitations and high resting heart rate, there doesn’t appear to be anything wrong. They don’t want to try any intense treatment unless it starts interfering with my daily life but they did recommend trying beta-blockers to help regulate my heart rate. Because beta blockers can make you tired, the cardiologist said I wouldn’t have to take them all the time but could try taking them whenever I start getting palpitations.
My GP has already filled a prescription for me so I guess I’ll give them a go once they’re ready. Whether this is related to my IBD or not, I don’t know, but it wouldn’t be too much of a stretch to think so as IBD can effect many parts of the body, not just the bowel. I’ll update again on this after I’ve been taking the beta blockers for a bit.
In other news, I’m going to flying to the Netherlands later this week so expect a post about that later next week. I’ll be sure to take note of how going through security goes this time compared to last time (hopefully, it’ll go just as smoothly).
I went to a Crohn’s & Colitis UK coffee morning today with my mum. It was good to meet new people, we talked a lot but there’s never enough time to speak to everyone. I hope to go to the next one near me though. I met someone who has had a jpouch for around ten years now, and I spoke to someone who came with their mum (like me) and who both have Crohn’s. A couple of them were also at the IBD open day last weekend too. I’ve always thought that these meet-ups are a good idea, they give you somewhere to talk freely and feel safe, as well as being part of a community that understands and doesn’t judge because they’ve been there. I know they’re not for everyone but I enjoy it.
In other news, I saw my surgeon last week and he’s very happy with how I’m doing. He said he doesn’t want to do anything now for at least another year, which is fine by me (two surgeries is more than enough for this year, thank you very much). He said I’ve got three options though; 1) I can have my stoma closed and try the jpouch again, 2) I can have my jpouch & rectum removed, a permanent end ileostomy formed and have a barbie-butt, or, 3) I can stay as I am with jpouch & rectum intact and loop-ileostomy. I am quite content to stay as I am for now, but eventually, I will want to go for option 2; permanent stoma and barbie-butt. I don’t want to go back to the jpouch because not only is it ulcerated, but I still have the perforation near the entrance, both of which make me not want to risk it failing again and having to have yet another surgery. I could stay as I am indefinitely but I think I’ll always feel like it’s not finished and I just want this to be sorted once and for all.
So, that’s it for now. Work is going well and I feel able to do more things and for longer. My appetite has returned with avengence so I’m eating like a horse at the moment. My weight is very slowly increasing so all good from where I’m sitting.
Case Western Reserve University School of Medicine has identified a fungus that is a key factor in Crohn’s disease. There is hope that this discovery, along with their finding of a new bacterium that is linked to the previous bacteria associated with the disease, will lead to new treatments and a cure.
From Science Daily:
“We already know that bacteria, in addition to genetic and dietary factors, play a major role in causing Crohn’s disease,” said the study’s senior and corresponding author, Mahmoud A Ghannoum, PhD, professor and director of the Center for Medical Mycology at Case Western Reserve and University Hospitals Cleveland Medical Center “Essentially, patients with Crohn’s have abnormal immune responses to these bacteria, which inhabit the intestines of all people. While most researchers focus their investigations on these bacteria, few have examined the role of fungi, which are also present in everyone’s intestines. Our study adds significant new information to understanding why some people develop Crohn’s disease.
The research found that the combined presence of the two bacteria, Escherichia coli and Serratia marcescens, and the fungi Candida tropicalis was much higher in fecal samples of people with Crohn’s compared to those without the disease.
Test-tube research by the Ghannoum-led team found that the three work together (with the E. coli cells fusing to the fungal cells and S. marcescens forming a bridge connecting the microbes) to produce a biofilm – a thin, slimy layer of microorganisms found in the body that adheres to, among other sites, a portion of the intestines – which can prompt inflammation that results in the symptoms of Crohn’s disease.
To learn more about the first time a fungus has been linked to Crohn disease in humans, read more at Science Daily or find the research here through Case Western.
Post link