#vetscience

Bender-scope
The microscopes of the future are all surly and a little bit hungover.
Current mood: “Bite my shiny metal a$$“
Zomb-hair
A very close-up scene from the hit TV series ‘The Walking Dreads’
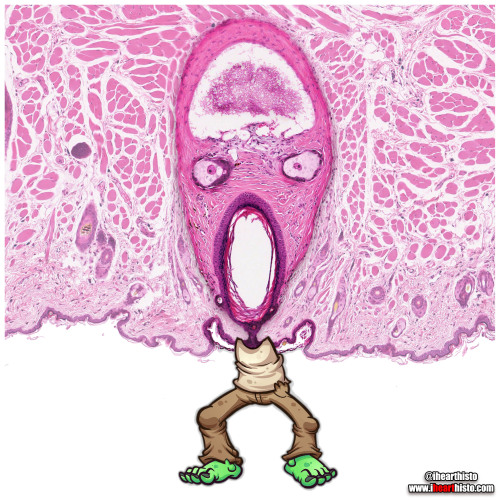
This is actually a vibrissae hair follicle from the face of a (a whisker).
Vibrissae are sensory hairs that are different from regular body hairs in the fact that they are surrounded by a blood filled sinus (z’s brain) and are associated with sensory neurons that have a distinct and representative pattern in the somatosensory cortex of the mouse brain. The fact that they are well mapped in the brain illustrates their importance in everyday behavior and survival - they are involved in things like detecting, orienting and sensing length of surfaces/objects and tracking (e.g. finding gaps in a maze and answering the question 'can my head fit through here?’).
Note also the sebaceous glands (z’s eyes) which secrete a lipid rich secretion called sebum for maintaining hair and epidermis keratin (keratin is the wispy stuff lining the skin at the bottom of the image and forming z’s lil arms).
The hair in this follicle is absent as you can see z’s wailing mouth is completely empty (where you might expect to see the shaft of a hair).
The closest things us humans have to vibrissae are the thick long hairs in our nostrils which are fairly sensitive to tickles (and make your eyes water if plucked) but more importantly provide a first line of filtration to prevent big particles from being inhaled into your nasal cavity.
#histology #science #anatomy #pathology #autopsy #pathologists #dermatology #halloween #hair #skin #zombie #dentalstudent #dentalschool #histotech #medlab #premed #meded #nurse #nursing #medschool #medstudent #medicine #vetscience #vetschool #histotechnology #histologia #histo #pathArt #vetstudent #ihearthisto
Post link
Surgery Rotation
My final rotation of the year! It seems like yesterday that I was following a hand drawn map of the hospital to locate the ophthalmology room for my very first rotation. How far I’ve come!
On this rotation we began with a small group of four students (rather than the usual eight) which was then divided in half, with two students beginning on soft tissue and the other two on orthopaedics. I was assigned to soft tissue surgery for the first week and it was hectic! My buddy and I were run off our feet trying to complete the work of four students. We arrived at 7:30 each morning and didn’t leave until after 7:00 at night when our patient records were completed. Once home, our evenings were spent frantically researching surgical procedures to avoid looking like complete idiots when the specialists inevitably quizzed us the following day.
Students were assigned to cases and responsible for collecting a history during the initial consultation with the owner, performing a physical examination, scrubbing into the surgery, writing a detailed surgical report, looking after the patient in hospital, administering medications, overseeing wound care, recording vitals and the progress of recovery, and eventually discharging the patient. Our ultimate goal was to get our patients through all of those stages and discharged as quickly as possible, to minimise the number of animals in our care and allow us to leave the hospital at a semi-reasonable hour each day.
Although being a group of just two students meant that we had an insane workload to keep on top of, we did get special treatment in the form of being allowed to scrub into almost every surgery! Students in previous groups were lucky to scrub into five surgeries during the whole rotation, whereas I scrubbed into ten just in the first week! Even so, being specialist surgery, our job primarily consisted of passing surgical instruments and cutting suture material (which was never quite the right length). One day towards the end of the first week, the surgeon surprised me by letting me place two sutures: a simple interrupted and a cruciate. That was two more than my fellow student, so I counted myself lucky!
During the first week, I was involved with a huge variety of soft tissue cases (prepare for big words) including an abdominal hernia repair, ventral bulla osteotomy, two dermoid sinus removals, multiple wound repairs, adrenalectomy, thyroidectomy, melanoma removal and skin flap, tongue biopsy, emergency plication to correct an intussusception, gastropexy, and ovariohysterectomy.
The most memorable case from this rotation was a soft tissue sarcoma removal from the hind leg of an elderly Golden Retriever. The surgery was performed on Monday and I arrived early the following day to find her leg very swollen. Over the week, the leg continued to swell and her condition steadily declined. By Thursday her breathing was laboured and I could hardly hear a heart beat. Our patient was transferred to the ICU to spend the night in an oxygen tank. The following morning she was much the same, still struggling for each breath. The vets had tentatively diagnosed her with von Willebrand Disease, an inherited clotting disorder caused by a defective or deficient protein. This meant the swelling in her leg was likely pooled blood as a result of uncontrolled bleeding from the surgical site. The disorder had never been detected previously and so it was an incredibly unfortunate and unforeseen complication. On Friday evening I went to check on her before heading home and reached the ICU just as someone yelled, “SHE’S ARRESTED!”. The emergency team sprung into action and began CPR. Her owners were contacted and the decision was made to let her go. It was a devastating end to what should have been a simple mass removal. Everyone involved was deeply affected by her death.
At the end of the first week, the resident came to see us in the student tutorial room. He told us we had done a fantastic job and he really appreciated our help. The hard work of final year students is often taken for granted, so the few times people have acknowledged and appreciated my efforts have really stuck with me!
Just as we were beginning to feel comfortable with soft tissue surgery, Monday came around and it was time to switch to orthopaedics. New surgeries, new patients, new team. At least I still had my student buddy for support and entertainment. There was an interesting mix of cases on orthopaedics, including bilateral hip dysplasia, intervertebral disc disease, two medial patellar luxations, shoulder arthroscopy, stifle arthroscopy and joint tap, and many tibial plateau levelling osteotomies.
Over the two week rotation, we had several tutorials on wound management, brachycephalic airway syndrome, neurology and fracture management. On the last Friday we had a short exam, followed by an orthopaedic cadaver lab, where we practiced our surgical approaches to the hip and stifle joints, and performed a femoral head ostectomy (a procedure in which the head of the femur is cut off to remove the hip joint).
The last surgery finished late on Friday and the hospital was eerily quiet. It was the strangest feeling saving my final reports, packing up my belongings and preparing to leave the hospital for the last time. The four of us didn’t really know how to react. We congratulated one another on finishing and headed home in stunned disbelief, unsure whether to laugh or cry. We didn’t have much time to process these feelings before our minds became consumed with panicked thoughts of the impending exams. It was time to put our heads down and bums up for one final push to the finish line!
Post link