#midwife




Ah yes,bugs,bugs and bugs
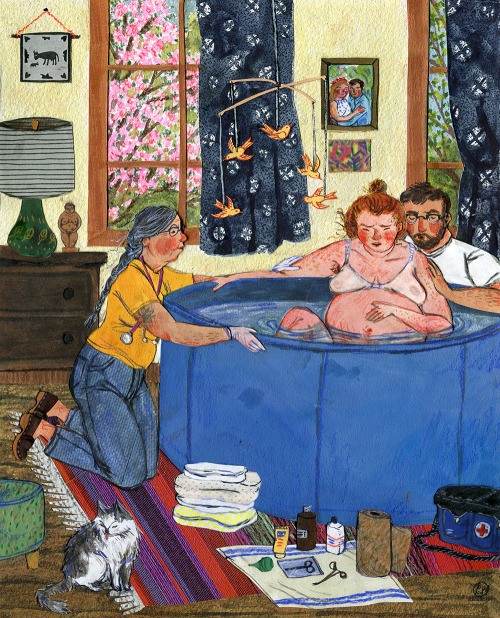
“BIRTH”
For March in the Taproot Magazine 2016 calendar.
Watercolor, collage, colored pencil. Phoebe Wahl, 2015.
Post link




Today is the International Day of the Midwife
The role of priestesses and women physicians who helped during childbirth in ancient times is extremely important. However, it has not been studied enough.
Giving birth to a child is taking a life from Death's hands and bringing it into the World. It is, thus, a combat, a battle in which a woman’s own life is put at risk. The patron divinity of birth is Tlazolteotl, Lady of Filth, who inspires sinful thought into people, which leads us to sex, and sometimes to error and wrongoing. Tlazolteotl is also the great purificator, who cleanses all that is dirty and regenerates the cycles of life.
You can find prints of the Temple of Tlazolteotl in my Etsy store! Click here!
Molar Pregnancy (Hydatidiform Mole)
Molar pregnancy is an abnormal form of pregnancy in which a non-viable fertilized egg implants in the uterus and will fail to come to term (will not develop into a child). Instead, the cells divide and replicate into a growing mass (mole) of non-foetal tissue.

Molar pregnancy is a gestational trophoblastic disease in which a non-viable egg grows into a mass (tumour) in the uterus that has swollen chorionic villi.

- Can develop when a fertilized egg does not contain an original maternal nucleus.
- Usually contains no foetal tissue.
- Characterized by the presence of a hydatidiform mole (or hydatid mole).
- Approximately 20% of women with a complete mole develop a trophoblastic malignancy (malignant disease // cancer)
Complete hydatidiform moles have a 2–4% risk of developing into choriocarcinoma in Western countries and 10–15% in Eastern countries, and have a 15% risk of becoming an invasive mole.
Molar pregnancies make up 1 in 1,000 pregnancies in the US and up to 1 in 100 pregnancies in parts of Asia.
Symptoms
- Vaginal bleeding- molar tissue separates from the decidua, causing bleeding.
- Uterus may become distended by large amounts of blood, and dark fluid may leak into the vagina.
- Hyperemesis - severe nausea and vomiting due to very high levels of human chorionic gonadotropin (hCG).
- Hyperthyroidism - thyroid gland is stimulated by the high levels of circulating hCG or by a thyroid stimulating substance (ie, thyrotropin) produced by the trophoblasts.
Partial mole
Partial moles do not generate the same clinical features as a complete mole. Patients instead present with signs and symptoms consistent with an incomplete or missed abortion, including vaginal bleeding and absence of foetal heartbeat.
Maude E. Callen Nurse & Midwife
Callen moved to Pineville, South Carolina in 1923, where she set up practice. She was one of only nine nurse-midwives, at the time, in the area. Callen operated a community clinic out of her home, miles from any hospital. She provided in-home services to “an area of some 400 square miles veined with muddy roads”, serving as ‘doctor, dietician, psychologist, bail-goer and friend’ to thousands of desperately poor patients.
It is estimated she delivered between six hundred and eight hundred babies in her years of practice. In addition to providing medical services, Callen also taught women from the community to be midwives. In December 1951, Life magazine published a twelve-page photographic essay of Callen’s work, by the celebrated photojournalist, W. Eugene Smith. Smith spent weeks with Callen at her clinic and on her rounds. The photos were visually arresting, both as a haunting record of the time but also as ongoing testament to the power of nursing and midwifery to effect social change.
Post link
Midwifery linked to better birth outcomes in state-by-state “report card”
Midwife-friendly laws and regulations tend to coincide with lower rates of premature births, cesarean deliveries and newborn deaths, according to a U.S.-wide “report card” that ranks each of the 50 states on the quality of their maternity care.
The first-of-its-kind study found a strong connection between the role of midwives in the health care system – what the researchers call “midwifery integration” – and birth outcomes. States with high midwifery integration, like Washington and Oregon, generally had better results, while states with the least integration, primarily in the Midwest and South, tended to do worse.
As with most population health studies, the statistical association between the role of midwives and birth outcomes doesn’t prove a cause-and-effect relationship. Other factors, especially race, loom larger, with African-Americans experiencing a disproportionate share of negative outcomes. However, almost 12 percent of the variation in neonatal death across the U.S. is attributable solely to how much of a part midwives play in each state’s health care system.
“Our results show that families experience better outcomes when midwives can practice to their full capacity and are part of the system,” said Saraswathi Vedam, an Associate Professor in the Department of Family Practice at the University of British Columbia, who led the team of U.S. epidemiology and health policy researchers responsible for the study, published Feb. 21 in PLOS ONE. “In marginalized communities in the U.S., where the health system is often stretched thin, expanding access to midwives and increasing their responsibilities could be a feasible strategy for improving maternity care.”
Post link

[image: the card I carry with to explain epidurals during labor, created by Penny Simkin]
I had a few requests for me to share my epidural informed consent ‘script’, so here it is in it’s MOST general version. Please remember that this is just an idea of what I might say, and it would definitely be different when I am with a laboring person, as I take their specific health and priorities and concerns and personality into consideration when I discuss this with them. This script is for someone who is undecided during labor about whether or not they want an epidural and is asking for more information.
*Of note: I don’t bring pain medication up without them starting the conversation unless I see them truly suffering. If I bring it up and they say no, I don’t bring it up again.
The conversation usually includes a few parts:
- Explaining what an epidural is and how it works
- Explaining the process for inserting the epidural
- Discussing risks, benefits, and alternatives
- Reviewing everything, answering questions, and then stepping out of the room to give them time to discuss if they would like that.
- Occasionally it may include offering a vaginal exam ahead of time if they think the information gleaned from the exam would change their decision
“I remember from your birth plan that you didn’t want to talk about pain medication unless you brought it up yourself - now that you’ve mentioned that you might want an epidural, do you feel like you’d like to talk about it? There’s no rush since I KNOW that you can do this and ARE doing this in the exact right way for you right now.”
If yes, I continue.
“Epidural anesthesia is a pain medication that numbs you from here [show them the top of the uterus/diaphragm area] down to your toes. Everyone experiences them differently, so some people are completely numb and cannot even move their legs, while most people have some control over their legs but are numb enough to not feel the intensity of the contractions any longer. While you won’t feel the intensity, you will still likely feel the pressure of contractions or of the baby’s head as the descend in your pelvis, and you will still feel touch to the skin. You will definitely feel the baby’s head coming out, and that may be painful or intense even with the epidural in place. Our anesthesiologists usually do an epidural that allows for your legs to move, and so we will definitely help you into whatever position you need - sitting up, lying down, squatting, hands-and-knees, lying on your side - as long as you are still in the bed. It’s not usually safe to try standing with the epidural since most people don’t have enough sensation in their legs to hold their weight.
“The way they place the epidural is they have everyone but one partner/doula/support person step out of the room and you sit at the edge of the bed with your shoulders slumped over. The anesthesiologist will give you a numbing shot to the skin on your low back which some people say is the most painful part of the whole ordeal - it feels like a bee sting. Once that area is numb, they insert a larger needle into the epidural space, in your spine. [I carry an illustration of this to explain what I mean.] Then just like an IV in your arm, a tiny plastic catheter (tube) is threaded into that space and the metal needle is removed. The epidural medicine drips in a small amount at a time through the catheter. This way we can give you more or less medication at any time depending on what you want or need. Sometimes we will increase the medication if the regular rate isn’t strong enough, or we will decrease if you need more sensation to move or push. It usually takes about 15 minutes to place the epidural and 15 minutes for it to start working.
“In order to have an epidural placed you will need an IV running fluids through your arm, continuous fetal monitoring, and a urinary catheter since you won’t have enough sensation to empty your bladder yourself.”
When it comes to talking about pros and cons I talk specifically about each person’s scenario instead of more generally, since the person I’m talking to is in labor! They don’t have much ability or desire to be thinking about anything that isn’t directly pertinent to them. Because of this I will discuss the epidural’s effects on the part of labor that they’re in now vs the future, but ignore the past. As in, if they’re in active labor I won’t talk about how an epidural might slow down early labor, but I might talk about it’s effects on pushing. For example:
“At this point you are in what we call ‘early labor,’ which means that your labor is still ramping up. It doesn’t mean that early labor is necessarily easier or that you will be in this place for much longer, but I have seen labors slow down when people get an epidural at this time. If that happens, we will talk about trying to stimulate your labor again either by position changes (though slightly limited in bed), nipple stimulation, membrane sweep, or pitocin. If you are coping well and able to go another hour without pain relief, I would recommend that we continue without. However the minute you tell me you have decided on epidural pain management, I will call the anesthesiologist. You are the only one who knows what’s right for your body.”
Another option for someone in active labor:
“At this point in your labor it’s unlikely that your contractions will slow down if you get an epidural, and in fact it’s possible that the relaxation of your pelvic muscles that comes with an epidural could allow baby to descend more and help to open your cervix with the pressure of their head. There’s no knowing what will happen either way.”
“The main risks to an epidural are the possibility that:
- Your contractions may space out [discuss what this would mean for their labor]
- The possibility of a postpartum headache (this headache happens to about 1 in 100 people and is treatable with pain meds, but is still a very frustrating experience in the postpartum period)
- The possibility that your blood pressure will drop and therefore your baby’s heart rate will slow (if this happens you can expect us to move you from one side to another, give you a ‘bolus’ aka large about of IV fluid, and maybe give you oxygen through a mask. Sometimes this can be scary because many Drs & RNs will come into the room all at once to address the issue. Though this may seem scary, when it is treated with the usual measures, it does not cause harm to baby or increase the risk for cesarean birth.)
- The possibility that the epidural won’t work at all or will have a small ‘window’ in which the epidural doesn’t work. If that happens our options are to grin and bear it, to try boosting the dose, or to take it out and try replacing it entirely.”
Here is a more extensive chart from LaborPains that I bring out sometimes when people are interested/in the right mind space to discuss further:

“The research is ambiguous when it comes to whether or not the medications passing through the epidural will affect the baby as well as the laboring person. There are no known long term disadvantages for babies. Babies are much less affected by epidurals than other medications used in labor that are administered by IV.”
“There are other things we could use as well to support you in coping with these contractions:
- Nitrous oxide - laughing gas (aka gas and air)
- IV medications (Morphine, Stadol, Fentanyl, Nubain, Demerol)
- Hydrotherapy - hot water in the tub or shower
- Sterile water injections - local pain relief without medications for back pain
- TENS units
- Massage, position changes, labor support”
See my post going into depth on those topics here.
“What questions do you have? Would you like me to step out for a moment so you can discuss this with your partner/doula/support person?”
Occasionally, if I think it would be useful, I will offer a vaginal exam before an epidural. For some people going through transition, the knowledge that they are close can give them some very needed encouragement. Vice versa, the knowledge that the cervix has not changed in many hours can also give people the information they need to decide that they would like an epidural.
“Would you like a vaginal exam before you decide on whether you would like pain medication or not? Many homebirth midwives will almost never use vaginal exams since they are quite right in thinking that vaginal exams don’t change the course of labor. However, in a hospital setting things change. There are interventions like epidurals to be considered, and a vaginal exam can give useful information to someone deciding on using an intervention. The exam itself IS an intervention in its own right. The information derived from a vaginal exam may tell us what stage of labor you are at right now. It does not tell us what will happen in the next 5 minutes (I’ve seen people dilate from 5cm to 10cm in 5 minutes) or in the next 5 hours (I’ve seen people be fully dilated for 5 hours before starting to push or giving birth). A vaginal exam is not required before you get an epidural, though. If you know for sure that’s what you want right now I will call the anesthesiologist right away.”
Resources:
Pain Medication Preference Scale - by Penny Simkin, for use before labor
https://www.ncbi.nlm.nih.gov/books/NBK279567/
Some of my fav music releases of 2020 that have gotten me through the year.
Listen to the playlist on Spotify|Soundcloud|YouTube
Post link