#type 1 diabetes
Friendly reminder from a type one diabetic to NOT use the “OMG I’M GONNA GET DIABEETUS” jokes as a response to anything (pictures of unhealthy food, favorite fanfictions, etc.) because:
1) It’s pretty offensive. I’m not overly offended personally because this joke doesn’t Target type one diabetes, but type two (and type one) diabetes imposes serious health risks. It’s not ok to make fun of that.
2) It spreads misinformation. Type one and type two diabetes are very different, but you don’t get either type from one unhealthy meal. Furthermore, I don’t need people who only know the diabeetus meme telling me “You can’t eat that! You’re diabetic!”. I promise I understand how my disease works.
3) It’s 2017. The joke has died out, I promise!
I never catch a cold, I immediately catch my death.
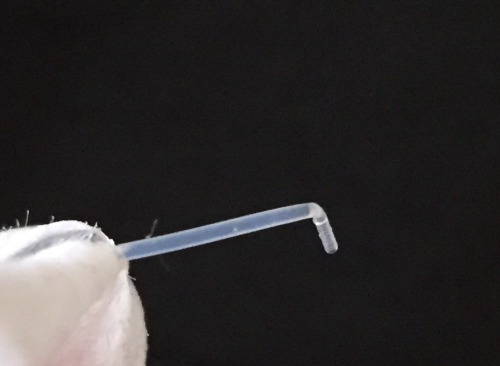
Why does this keep happening??? I use angled sets to avoid kinking!
I guess it must be all my superior muscle mass and adamantium skeleton getting in the way…
Post link

You know, I was trying to actually cook like a successful grown-up.
Hi, all–sorry I’ve been so long.
So, do I have news for you! I officially have chronic condition #2, thought to be autoimmune. Now, in addition to attacking my pancreas, my immune system has decided to revolt against my skin. At least I’m special; less than 1% of the population apparently has this condition. Thing is, while rare toys, cards, books, or collectibles may be great, rare diseases are far less so.
What surprises me is how much more of a toll this diagnosis was taking on my self esteem than has diabetes this past week. For better or for worse, diabetes is an invisible illness. It has far more of an impact on my life than skin changes, but I can hide my pancreas problems if I so choose (though I usually don’t). You can’t hide a skin condition, and it doesn’t make you feel pretty. It makes you feel strange, and it seems harder to reclaim as a positive in the way that I own my “cyborg parts” as a part of my diabetic identity.
The good news is, with the diagnosis and proper treatment, I’m getting better.
I like to imagine that my immune system is just so incredibly strong, though it may attack my body, it’s also some sort of superpower–maybe I’d be immune to a zombie contagion or nuclear fallout. Silver linings?

They’re here! The buttons are here! Donate to get yours before they run out and help me run out diabetes instead:
http://www2.jdrf.org/site/TR?fr_id=6292&pg=personal&px=10474618
Come on, guys! A month left to donate. These buttons are limited in quantity, and all you have to do is donate to help find a cure for type 1 diabetes! It’s a win-win! Just include your mailing address when donating:
http://www2.jdrf.org/site/TR?fr_id=6292&pg=personal&px=10474618


Like this cutie little button, designed by yours truly? You want one? Easy!
This year, to raise money for JDRF, I’ll be sending one of these little guys to every person who donates to my page. Link below!
http://www2.jdrf.org/site/TR?fr_id=6292&pg=personal&px=10474618
Make sure you include your name and mailing address when donating!
If it goes well, I might make other diabuddies for you all! Pens, meters, etc…give me a reason!
Shouldn’t have been surprised by this advantage of working at a toy company: when your pump runs out of juice, everyone at work has triple A batteries on hand!
My blood sugar is taking forever to come down and I don’t know why…

Dear stranger from dance,
I appreciate your asking about my pump, how it works, why I wear it. However, when you watched me check my blood sugar, your comment registered not interest and affection, but pity. In fact, you were’t even subtle. As I licked the small drop off the top of my finger, a routine part of my life, you said:
“That’s so sad.”
You didn’t even bother to whisper. You said it to my face, as if I should agree. Somehow, I was meant to validate your sympathy. Yet, here’s the thing–I’m not sad, and even if I were, your opinion of my condition would not affect that.
People like me–people with disorders, illnesses, and disabilities–do not exist as receptacles for your empathy. You don’t get to feel elevated for your understanding nods and soft tones. I don’t need soft tones. I won’t break like a glass when your voice hits a high note. I do need your understanding, like any other human being.
So, no I’m not sad. My life is just different from yours. The night you said that to me I danced until midnight, went for drinks with friends, and collapsed in bed just in time to get enough sleep for a party the next day. I checked my blood sugar a few more times and changed a pump site in the midst of all that, yes, but that’s just my normal. And that’s okay.

Seriously, I had multiple Finding Dory band-aids across my butt today so I didn’t stain my dress :(
Sorry I’ve been so long in writing-being an adult is time consuming! But, long post coming up, so maybe y'all can forgive me.
My dad is fantastic. For the past few months worked to raise thousands of dollars for the JDRF Burlington ride by…selling his body. To clarify, he came up with this awesome fundraising idea: if you donated over a certain amount, my dad would wear a (temporary) tattoo of whatever you wanted during the ride. He looked like a sponsored NASCAR driver! Though it may just sound silly and fun, it worked-he raised over $10,000 for research.
Lesson to learn: my dad is the coolest, he loves me a lot, and people love silly tattoos on grown men.
My mom and I went up to volunteer at the ride as well. It was an awesome experience, and if you ever get to go, you should. There’s something really comforting about going somewhere were all the food is carb counted; it means someone understands. It’s great to connect with families from all walks of the diabetic life and hear about new technologies. Yet, the most amazing thing is seeing how much everyone really cares for you. How much they are willing to take on, volunteer, and donate so you can be healthy.
Plus, the all-T1D bike team is very, very cute.

^one of my dad’s tattoos, complete with insulin syringe instead of Cupid’s arrow
Picture this scene:
I’m casually at a bar with a friend. Said friend suddenly grabs my shoulder and says, “You are suchan inspiration.”
Really? How?
I appreciate the compliment, I suppose, but it’s false. What seems to make me “inspirational” is simply my ability to function as a human being. The fact that I do everything like anyone else does not make me special just by virtue of my illness.
What this implies is that living with a disease or disability is so incomprehensibly difficult that we should be admired simply for existing.
Living with a disease is not fun. It does not make you “special.” There’s nothing wrong with claiming your individuality as a sufferer, but it’s incredibly different when others claim it for their own purposes, be it self-aggrandizement, fantasy (more to come on that topic soon), or “inspo.”
Tell ya what–you are inspirational because you do awesome things. You follow your passion, you have ideas, you kick ass. Proper pancreas or lack thereof is not a factor in fabulousness!
…if it ain’t got that swing!
I dance a lot. If you can’t find me at any given time, it’s probably because I’m twirling somewhere. When you’re a follow in swing dance, you have to be a “zen master.” Attuned to my partner’s cues, my mind goes blank. If I think too hard about what my body is doing, I stiffen and the dance falls apart. Yet, I’m still completely focused, aware, and ready in motion.
It’s a lot like that with diabetes, too. If I think too hard and become neurotic about my BG, things go wrong. I overcorrect, under eat, and dip too low. If I’m not aware at all, well then…no one likes DKA.
Like dancing, diabetes relies on communication between you and your body. And yeah, sometimes you trip and fall or accidentally punch your partner in the face, but that’s okay. It happens!
Plus, dance (or any physical activity) is great for BG control and looking sexy. Representing that pump life!

Comprehensive Care for Gestational Diabetes
Women with diabetes need comprehensive care before and during pregnancy. The Diabetes and Pregnancy Program (DAPP) at UC San Diego Health, the only one of its kind in the San Diego Region, cares for the diverse population of women with diabetes in San Diego County.
DAPP is designed to provide specialized care to patients with diabetes through a multidisciplinary approach, following the California Diabetes and Pregnancy Program guidelines.
“Patients with type 1 or type 2 diabetes, or those who have recently been diagnosed with gestational diabetes, require a team of specialists to assist with a healthy pregnancy and optimize the outcome for both the patient and baby,” said Sandy Ramos, MD, director of DAPP and perinatologist at UC San Diego Health.
“For example, working with a specialist to manage blood sugar before and during pregnancy can decrease the risk of complications and make it more likely that the patient can carry the baby to term.”
Ramos and Kristen Kulasa, MD, endocrinologist at UC San Diego Health, elaborate:
Question: How common is gestational diabetes and what are the complications?
Answer: Approximately one in five women delivering babies in San Diego County begin their pregnancies with diabetes, and others develop gestational diabetes during pregnancy. These women are at risk for complications during pregnancy and after delivery, including high blood pressure, eye disease, kidney disease, too much weight gain, severe hypoglycemia (low blood sugar) and diabetic ketoacidosis (DKA).
Their babies are also at increased risk for complications, including macrosomia (high birth weight), higher rates of miscarriage and stillbirth, birth defects, delivery complications and jaundice.
Q: What type of services does DAPP provide?
A: DAPP includes six certified diabetes care and education specialists (DECS), nutritionists and social workers under the direction of two maternal fetal medicine experts. The program provides care to approximately 500 patients with gestational diabetes, 120 patients with type 2 diabetes and 40 patients with type 1 diabetes per year.
As a clinical program in the region’s only academic medical center, DAPP provides leading edge diabetes care from preconception to postpartum, utilizing the latest technology available, including the use of sophisticated insulin pumps and continuous glucose monitoring.
For example, the DAPP team has found success using “closed loop systems” to improve glucose control in patients with type 1 diabetes in pregnancy. This technology allows integration of information from the continuous glucose monitor to augment or “talk” to insulin pumps. This allows the insulin pump to increase insulin delivery if the glucose values are high or to decrease or even suspend insulin delivery if the glucose value is low.
With the aim of improving the maternal and neonatal outcomes of women with diabetes, patients are also given the opportunity to participate in clinical trials, such as the Medical Optimization of Management of Pregnancy with Overt Diabetes (MOMPOD) trial, a randomized clinical trial of Metformin as an adjunct to insulin for the treatment of type 2 diabetes.
DAPP provides primary obstetrical care for complicated patients with diabetes and is able to provide consultative services to co-manage patients with gestational diabetes.
Q: How are you addressing gestational diabetes with patients in terms of lifestyle interventions and medications available?
A: To treat gestational diabetes, we encourage nutrition changes to limit simple carbohydrates and recommend exercise. Most patients with gestational diabetes can manage their glucose values with these changes alone. If elevations persist, they can be treated with medicines like insulin and metformin. However, these lifestyle changes are important tools to continue to lower the risk of development of type 2 diabetes. Women who develop gestational diabetes have a higher risk of developing type 2 diabetes later in life.
Q: What research needs to be done to improve how diabetes is managed in pregnancy?
A: There are many new medications used for management of type 2 diabetes that haven’t been studied in pregnancy. The issue of safety of these medications needs further exploration in pregnancy. Additionally, technology, including blue tooth-enabled meters and continuous glucose monitors, commonly used in type 1 diabetes, need to be studied in other types of diabetes in pregnancy to see if they may be useful tools to improve the care of women with diabetes.
— Michelle Brubaker
Post link

I now finally have covid. Fml. Symptoms so far are very mild and I’m vaccinated 4 so here is hoping these antibodies work! Fucking hate this!!!


Some details of my outfit today