#doctor
Section #2 of Professor W.T. Eckley’s dissecting class, College of Physicians & Surgeons, 813 W Harrison St., 1898, Chicago
University of Illinois At Chicago Library of the Health Sciences University Archives
Post link
Sexualize spleens Sexualize spleens
Sexualize spleens
This story is wild but…
I’m posting this over here bc Talking about this gives me PTSD. Physically mentally takes a toll on me.
Breathing has become more. of a chore.
What happened to me 3 years ago was “Dr. Naderi” crushed my bones, caved them in, surgically removed my nostrils AND left me with a neurological breathing disease. in which He ditched me after surgery, lied, tried to cover it up, called me crazy and has sadly done this to more. I am not upset about the way it looks, I am upset about the fact that he removed unnecessary organs & didn’t tell me leaving me with a very serious condition.
- it almost felt like… a hate crime…??
It’s cost me so much & I went to court but Covid got in the way. Lawyers don’t want to take on any hard cases let alone any cases and yet Medical Malpractice is the 3rd Leading Cause of death!!!!!!!!!!!
I am sadly on disability now :(
Treatments have cost me a lot!!!! I wanna say 30k all together. Not to mention it takes me. out of work a lot.
Again, I’m finally speaking out, as I will continue to.
The doctors name is “Dr. Naderi” & he works out of Virginia.
….. Google & Google Reviews
Like @h3h3productions I wish ALIEN GANG were as big as Gerd Gang so they could all go pay a visit to this doctors Google Reviews or whatever.
I took screenshots of the reviews that sounded similar mine.
I started wearing masks bc of this 3 years ago & once Covid hit fortunately I had masks & access to PPE to help
I do have a lot of cute extra ones left fortunately bc I got extra in case. I also have a lot of cute other designs & items.
Google “Dr. Naderi” or Lexa Terrestrial ENS
to learn more about this.
And in no way am I saying to pursue some justice via Google reviews!
;p
#hair #masks #anime #nose #makeup #nosejob #nosefiller #ENS #rhinoplasty #pghartist #covid #plasticsurgery #awareness #trap #femalerapper #hiphop #blogs #stemcells #stemcelltreatment #lofi
#depression #anxiety #awareness
#plasticsurgeon #doctor #rhinoplastybeforeandafter #recovery #endhate #endviolence #spreadlove #yourebeautiful
(at Herndon, Virginia)
https://www.instagram.com/p/CLWoXg4h_QY/?igshid=1fm7l0xyip6f0
Post link

Dr. Drowzee: Alright, bend over (to self)
Pediatrics (neonates to school age; adolescence is another topic) is probably my least favorite specialty to deal with and they are one of the hardest to help at times with all the elements that go with the patient. Whether it is dealing with the sick child or the distraught parents, we must sift through the physical findings and the information from the parents to understand what is going on. This gets especially sticky when it comes to some upper airway complications in the younger group.
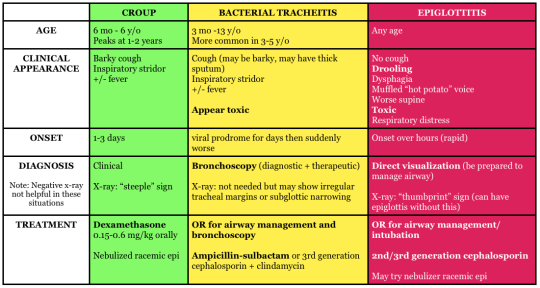
Two very common upper airway problems in the younger populations include Croup and Epiglottitis. Both can be dangerous, but require different management when treatment is concerned. This article will give you a brief overview of the pathophysiology, signs and symptoms, treatments, and key points to remember.
Croup
Pathophysiology: Commonly a viral infection (RSV, adenovirus, influenza A and B, etc.) of the upper respiratory system for ages 6 to 36 months. Major inflammation has occurred in the larynx, trachea, bronchi, bronchioles, and lung parenchyma; causing obstruction of the airway. As the swelling progresses supraglottic the patients with begin show signs of respiratory distress. Further along, the patient’s lower airway may begin to begin having atelectasis, due to the lack of air keeping the alveoli open.
Croup is a slow progression of inflammation. Noticing early that the patient has upper respiratory issue is key in the management. Due to the smaller airway of children, we must not hesitate to seat
Signs and Symptoms: The most common sign of croup will be the seal like bark with inspiratory stridor. With this means that the patient is in respiratory distress and quickly heading to failure. If you hear the seal like bark, check the lower lung fields for crackles, because possible atelectasis may have begun.
Commonly more serious during night, awakening them from sleep. Other signs to know include:
- Tachypnea
- Retractions
- Cyanosis
- Shallow respirations
- Fever
Treatment: Emergency treatment for croup is a humidified air and a dose of corticosteroids. If in further destress, racemic epinephrine will assist with edema. ETCO2 and O2 readings will help determine if there is retention of gasses, which may lead to acidosis. ABGs will be needed to confirm this as well.
Usually, patients will be able to return home to be monitored. Family should watch for difficulty breath and be using humified air. Antipyretics will assist in keeping fevers down as well.
Epiglottitis
Pathophysiology: Influenza type B, streptococcus pneumoniae or aureus may cause epiglottitis. The epiglottis is a small flap above the glottic opening, which is used to prevent foreign objects entering the trachea. When the epiglottis is infected, with will swell, narrowing the airway for the patient. Increased work of breathing may occur and soon my might have a patient in respiratory failure.
Epiglottitis is a more acute problem, with sudden onset and quick changes to mentation form the restriction of airflow.
Signs and symptoms: As the epiglottis swells, the child may begin to develop stridor. When stridor occurs, we must ask the question is this an object or is this medical. Other signs that might point you towards epiglottitis will be:
- Sore throat
- fever
- Odynophagia
- Drooling
- Irritability
- Cyanosis
- Tripoding or nasal flaring
Treatment: The most important thing with these patients is to ensure they have an airway. Do not try and examine the patient, especially if you are a paramedic on scene (Load and go). When gathering a medical history, it is especially important to ask for vaccination in the pediatric population. Today, Influenza vaccinations are given to children, but we do have a set population now that do not vaccinate their children. X-rays of neck will be done and a visual examination may be performed. Keep the patient calm at this time, further agitation may cause the airway to swell more.
Patient will commonly receive an antibiotic, such as ceftriaxone, to help with the bacteria. ET tubes may be places in severe cases and usually remain for 24 to 48 hours. Trachostomes may be required, if a ET tube cannot pass the glottic opening.
Key Points
- Both Croup and Epiglottitis can be dangerous to pediatric patients. If you have a child that has stridor and any signs of distress, they will need immediate attention.
- Out of hospital, assume epiglottitis and rule it out when you can. This load and go for you
- Croup X rays may show steeple sign, but epiglottitis won’t
Written by: MEDDAILY
Join me on Facebook!
The new strain of grain could grow anywhere, much to the horror of the few left alive in the endless fields of wheat that now seemed to cover the world.
Post link
I haven’t touched watercolors in about a year. Then I sat at a target food court and just absolutely went for it. Except the lettering because I am an absolute coward.
Post link
Anatomy lessons at St Dunstan’s

By J.H Lobey, 1919
The present picture shows the instruction of blinded or sight-impaired men in human anatomy.
Lectures in anatomy, physiology and pathology were given to blinded men at St Dunstan’s who were trained to become masseurs (Pearson, loc. cit.). Two of them are wearing spectacles, including the second figure from the left, who also has a burned face. The third figure from the left directs his eyes straight ahead of him but holds his hand on the skeleton’s left femur, much lower down. The teacher appears to be the woman in uniform and hat who is showing the insertion of the head of the femur into the hip joint. The instruction takes place in one of the canvas buildings erected in wartime on the terrace between the back of the house and the lawn
Starting clinical rotations can be overwhelming. If you’re like me, you may spend the first days stressing about where you should go, what questions are legit to ask and how you should behave. Most of the time you may have no idea of what your superiors are talking about and you just fake a smile and pretend you know exactly what you’re doing. Meanwhile it’s totally normal to feel lost during the first days of your arrival in a new care unit, it shouldn’t last and you should be able to get more comfortable with the team you’re working with and become more autonomous. Here’s how to get the most of your clinical rotations:
- ALWAYS introduce yourself when meeting with a new team : it will always be appreciated and people should be able to reach out to you if they need it
- TAKE NOTES and always keep a little notebook in your pocket! I actually own 3 (yes it may be a bit excessive) : one for patient’s history, one for personal notes and another one for definitions and scores
- Ask for feedback. The resident you’re shadowing may not necessarily think about giving you a feedback, or maybe he won’t pay enough attention to what you’re doing, and that’s why it’s better if you ask specifically for a feedback, especially when completing a task that you’ve been asked to do.
- If there’s a « down » moment when you don’t have anything to do, ask if there’s something you can do for help, even to other members of your team. Don’t hesitate to reach to the nurses or the other medical staff and ask for some teaching! I once spend an entire day with the nurses of my unit so I could learn how to properly draw blood.
- If there’s really nothing to do, use this spare time to study a specific subject, and ask your resident if you can present it to him : not only it forces you to study a subject, but you’ll also be able to actively recall it better
- Before seeing any patient alone, make sure you went through his medical history so you already know if there’s a specific topic you have to investigate more : be prepared for questions from your assigned residents/physicians!
- MAKE THE CALLS. I know, I know, making phone calls is SUPER SCARY (especially when you have to call chiefs and professors). However, I like to say that it’s like running : the more difficult it is, the more you should do it. Prepare what you have to say so you don’t loose yourself during the call, and force yourself to make the phone calls as often as possible. You’ll gain more and more confidence and you won’t be so scared anymore.
- NEVER be late.
- If you feel there’s something wrong (with you of with a situation) : talk to your assigned resident/physician. They know how overwhelming it can get, so don’t hesitate to reach out for help
- Bring snacks. And a big water bottle. Avoid drinking too much coffee.
- Being a medical student has many good sides : you can get a first hand-on experience with patients without huge responsibilities, it is the BEST time to make mistakes and ask « silly » questions ! If you don’t do this during this time, you won’t be able to do it later.
- Most of the time, you’ll feel like you know nothing, and you’ll forget about things you learned the day before. It’s normal. Don’t be too hard on yourself.
- Be patient. And LISTEN.
- ENJOY YOUR TIME ! Be curious about everything, make new friends, talk with your patients, see as many things as you can, because this is the only time where you can get all these possibilities!!
Peter Capaldi had said in interviews leading up to this season premiere of Doctor Who that we wouldn’t really get a sense of his take on the iconic character until episode 5 or 6. That is pretty standard in Moffatt’s world of doing things as Matt Smith‘s version of the time traveller took a bit to get into it. I was concerned about Capaldi’s tenure because Smith’s first episode had one of the greatest introduction of any character in all of TV towards the end. With Capaldi it all seemed rushed.
And then the last couple of episodes kicked in.
We started to really get a peak of the type of Doctor Capaldi was going to be with Listen. Then Moffatt gave us one of the best and most Doctor Who like episode in years with TimeHeist. Last week’s The Caretaker was very reminiscent of the types of adventures that William Hartnell(theFirst Doctor) used to go on.
So next up we have a trailer for this weeks episode Kill The Moon. It looks intriguing and very much in line with the Doctor that I love where he is in space dealing with the most ridiculous thing ever – yet it is the scariest thing as well.
Check out the trailer below and you bet your ass I will be there this Saturday watching this episode.
Hermione Norris(“MI-5,” “Wire in the Blood“) guest stars in “Kill the Moon,” premiering Saturday, October 4 at 9:00pm ET.
https://www.youtube.com/watch?v=CJyh8AI_M00
Original Article http://bit.ly/1vtVk5x